Neuroscience
Skull Fractures, Concussions, Contusions,
Hemorrhage, Loss of Consciousness, Coma
Rhawn Gabriel Joseph, Ph.D.


On TV and in movies, heroes, villains, and innocent bystanders, are often knocked upon the head, rendering them temporarily unconscious, after which they awake, good as new. But in reality, a knock upon the head sufficient to render loss of consciousness typically also causes brain damage. It is the injury to the brain which induces the unconscious state, and the longer the unconscious period, the greater is the damage to the brain. In fact, these bumps may also damage the skull, burst blood vessels, and cause the brain to slosh around inside the cranium causing extensive cerebral injury. Even "mild" head injuries can damage the brain, even without loss of consciousness.
Traumatic brain injury may well be as common as stroke as a leading cause of neurological injury and death in America and Europe . Well over a million individuals a years seek medical attention in the United States alone, and 500,000 require hospitalization, with 70,000 developing long term disabilities, and 2,000 remaining in persistent vegetative states. Almost half of such injuries are due to falls (especially in children and older adults), with assault, automobile accidents, gunshot and stab wounds comprising the bulk of the remainder.
The number of individuals who suffer significant head injuries is actually unknown, and is open to debate, as not all those who suffer head injuries, including even those suffering loss of consciousness, seek treatment. Moreover, children who are abused and beat seldom come to attention of authorities or medical personnel unless their injuries are life threatening or exceedingly obvious. In addition, men with supposedly "mild" head injuries, tend to downplay the significance of their injuries and are often reluctant to seek medical attention unless cognitive and physical functioning is significantly compromised.
Unfortunately, some physicians and emergency room personnel also down play the significance of "mild" head injuries, particularly when the patient appears to have more immediate and life threatening problems. And even if the patient's only complaint is head injury, if it is not life threatening or there is no evidence of loss of consciousness, medical personnel are likely to dismiss the injury as insignificant and/or to regard the patient's complaints as imaginary or related to a desire to file a lawsuit. Undoubtedly this is true in some cases. Nevertheless, frequently the majority of such individuals are not even involved in litigation (Barth et al., 1983; Merskey & Woodforde, 1972; Rimel et al., 1981). Moreover, sometimes the actual deficit is greater than the patient realizes (Prigatono et al. 1990; Waddell & Gronwall, 2004). Indeed, this attitude on the part of health care professionals is unfortunate, for as will be detailed below, even those with "mild" head injuries often suffer from prolonged neurobehavioral and affective deficits (Deb et al., 2012; Miller, 1993), including debilitating post traumatic headache (Zasler 2012), and among the elderly, significant cognitive decline including dementia (Luukinen et al., 2012).
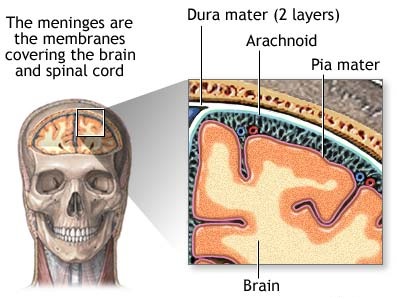
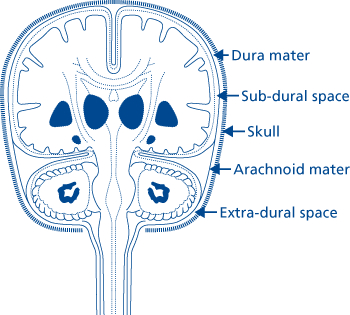
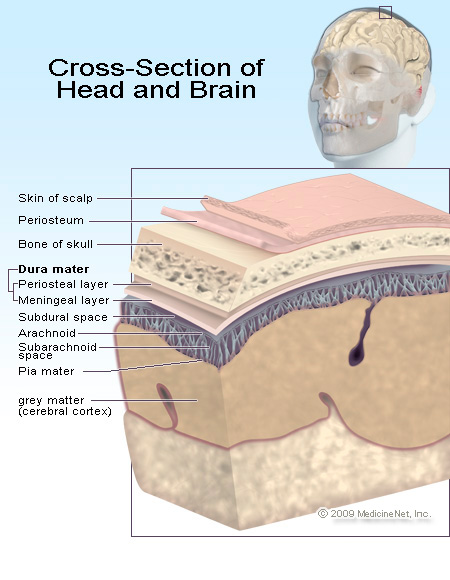
THE MENINGES
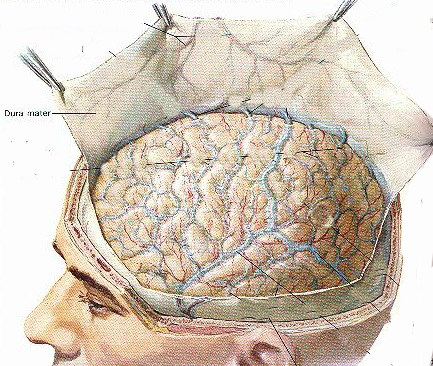
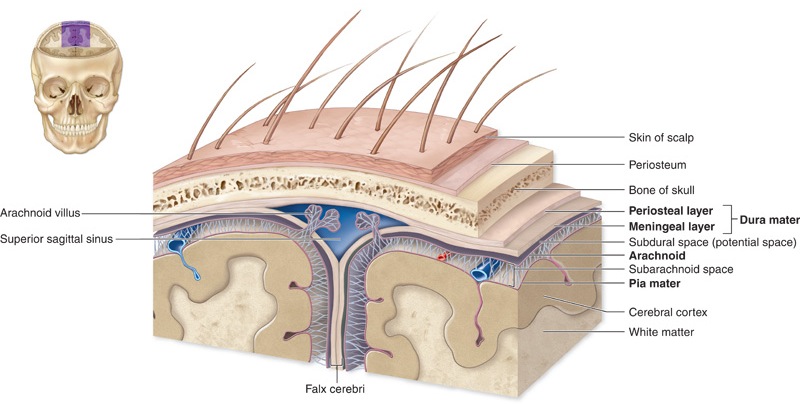
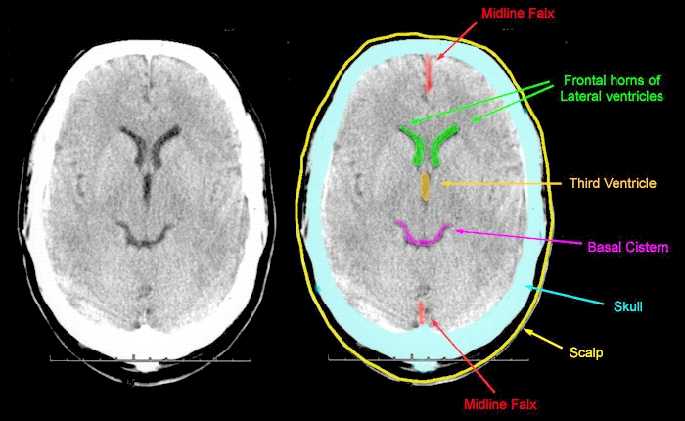
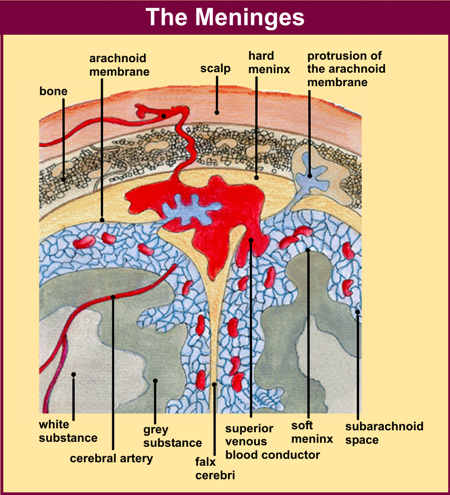
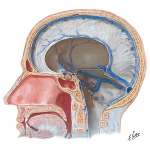
The living brain is a soft and delicate tissue with a rather compact consistency. The brain is protected by several outercoatings (i.e. membraines) which act as a cushion between it and the hard inner shell of the cranium. The inner most membraine is a sheer sheet of translucent material which actually adheres to the brain surface. This is called the pia matter.
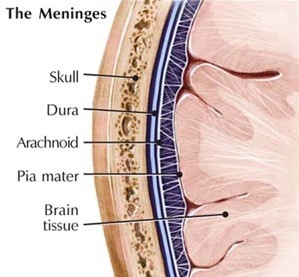
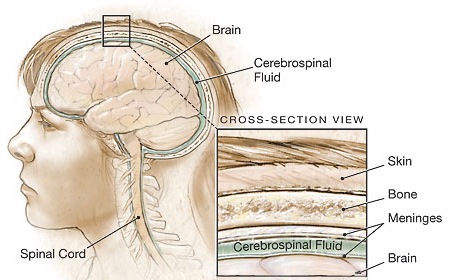
Lying above the pia matter is yet another very thin web-like fibrous membrain referred to as the arachnoid. The space between the arachnoid and pia matter is called the subarachnoid space through which circulates cerebrospinal fluid. Collectively the arachnoid and pia matter are called the leptomeninges.
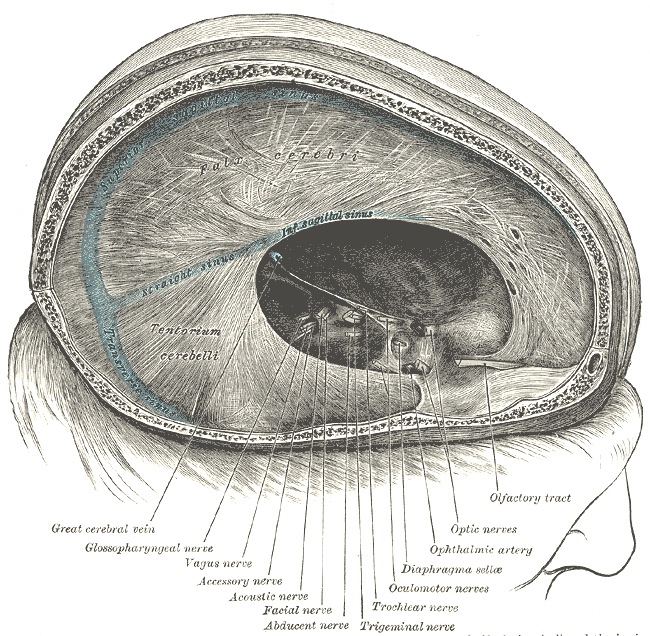
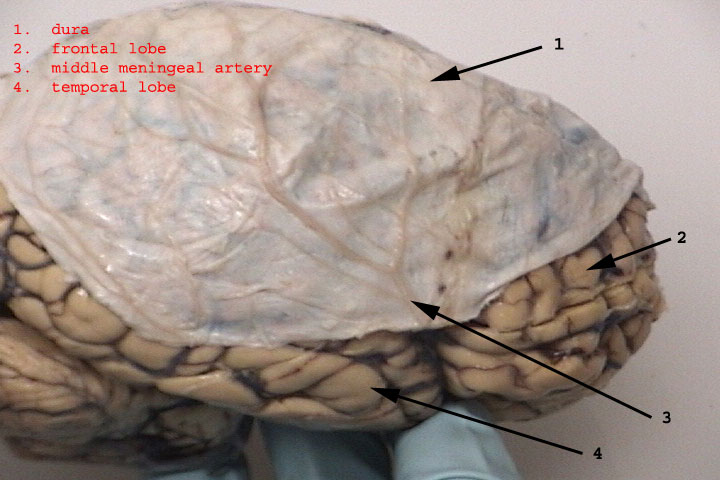
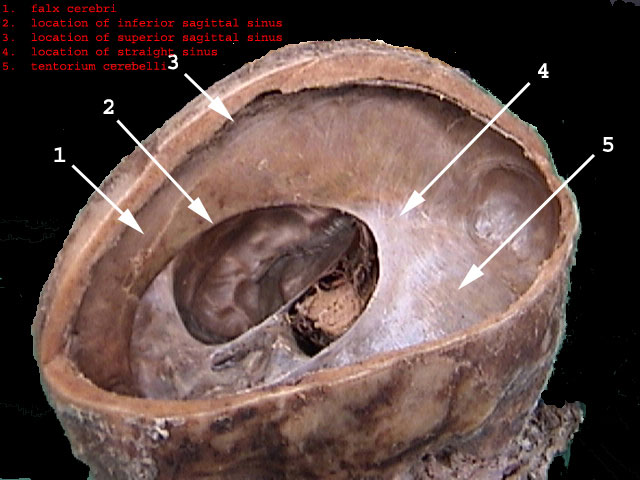
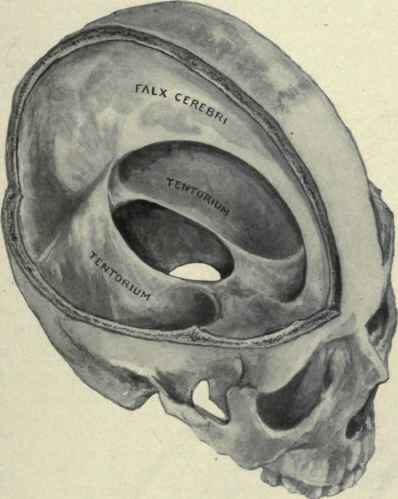
Sitting above the leptomeninges and partially adhering to the inside of the skull is a thick, tough, leathery-like membrain, the dura mater (i.e. "tough mother"). The dura mater is richly innervated by blood vessels, including the middle meningeal artery (which is sometimes subject to laceration following skull fractures creating a epidural hemorrhage).
The dura not only acts as a hard shield protecting the brain from the skull but forms a number of compartments which partly encompass and support various portions of the cerebrum. One major compartment is formed by the dura is the Falx cerebri which juts down between the cerebral hemispheres. The falx in turn gives rise (in a fan-like fashion) to the tentorium cerebelli upon which sits the occipital lobes and below which is the cerebellum. With certain types of head traumas, movement of the brain against the Falx and tentorium can causes contusions and shearing of cortical tissue.
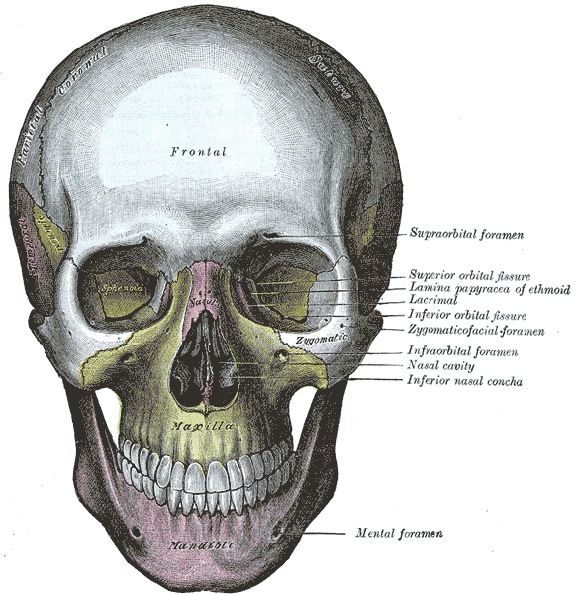
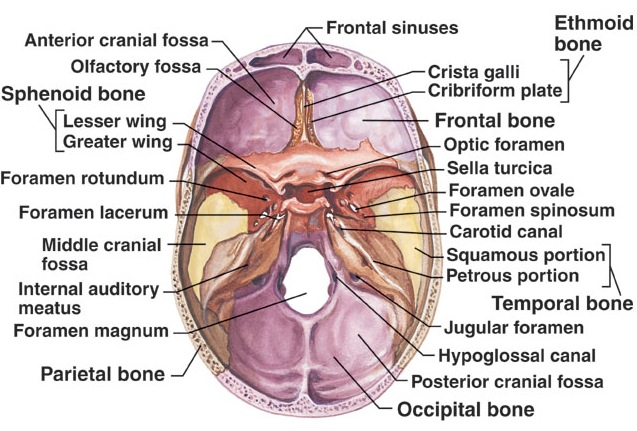
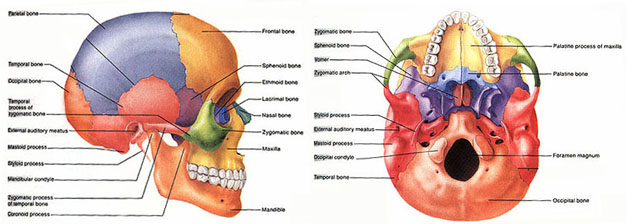
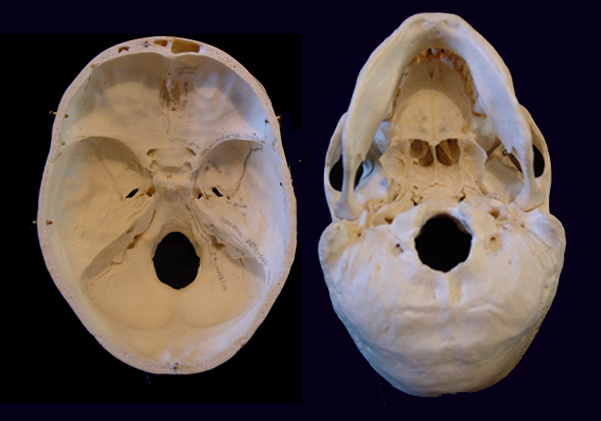
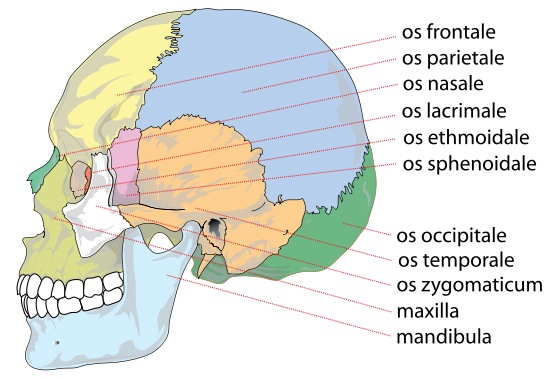
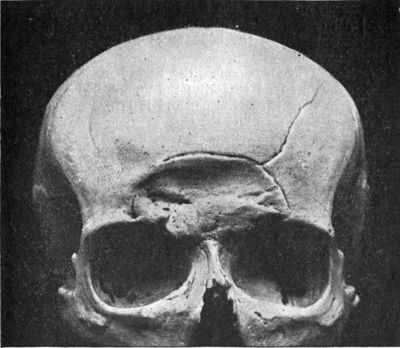
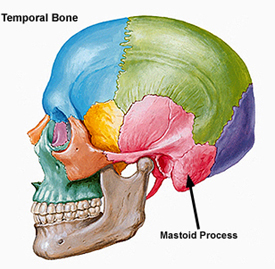
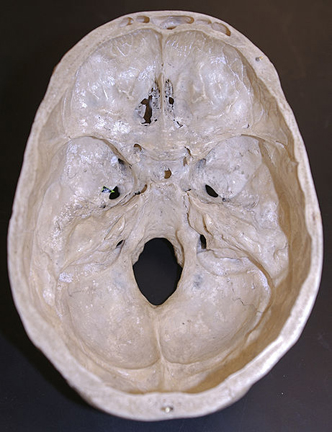
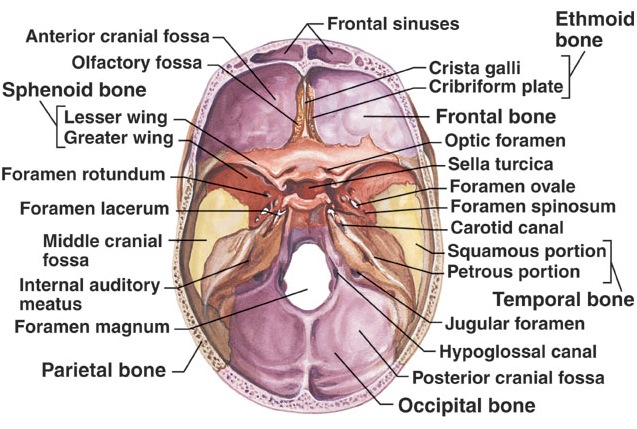
THE SKULL
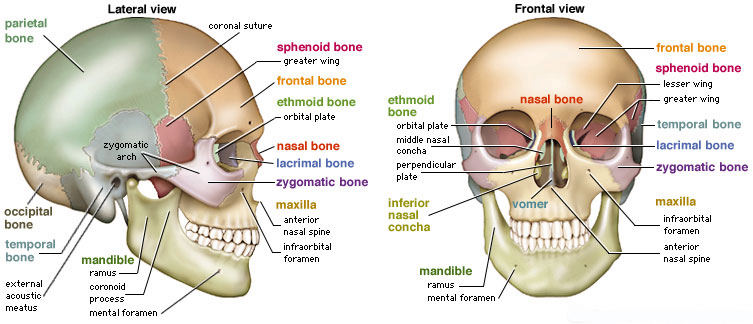
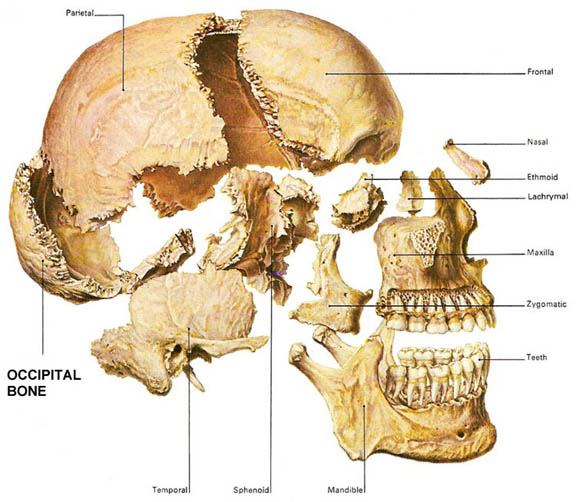
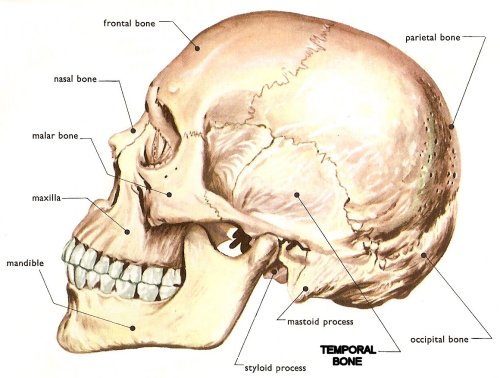
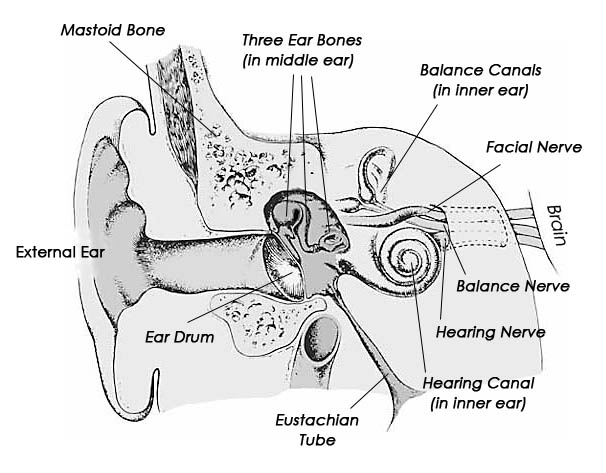
Completely encasing and supporting the brain is a thick bony covering which protects it from damage; i.e. the skull. The cranium is composed of several bony sheets; e.g. the frontal, parietal, temporal and occipital bones. The frontal bone constitutes the skeletal framework for the forehead (including the orbits for the eyes) and is joined to the parietal bones (the bulging topsides of the skull) by the coronal sutures. Comprising the lower and lateral portion of the cranium including parts of its floor are the temporal bones which also house the structures of the inner ear. The occipital bone makes up the lower posterior portion of the cranium.


If the skull is struck by a blunt object, the impact area will flatten with stress oscillating outwards laterally --like a rock hitting a pool of water. If sufficient pressure is applied the skull will fracture. Usually the break occurs at the site of impact.
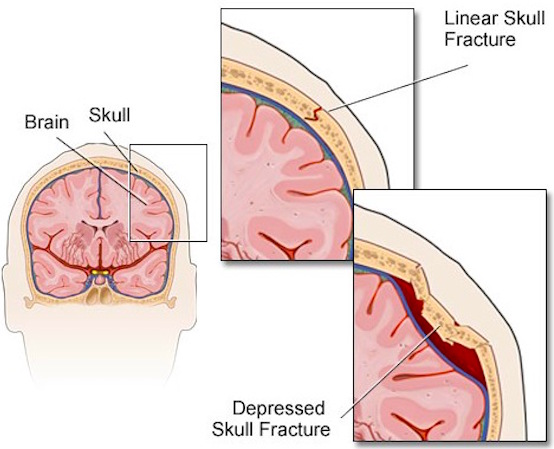
Skull fractures are of three types, depressed, linear or basilar. Basilar fracture are relatively uncommon whereas approximately 75% are linear, the remainder being depressed. However, some patients may suffer all three types of fractures.

Typically, if the skull is fractured, the underlying brain has been injured. In general, head injuries are also considered as either closed, or open if accompanied by scalp laceration and/or if the fracture extends into the sinuses or middle ear.
BASILAR FRACTURES
Basilar fractures often extend into the base of the skull and are difficult to detect unless quite severe. However, existence of a basal skull fracture may be indicated by cranial nerve damage or hormonal-endocrine abnormaltiies (such as from damage to the pituitary). Fractures near the sella tursica (at the base of the skull) may tear the stalk of the pituitary such that in consequence diabetes, impotence, and reduced libido may result.

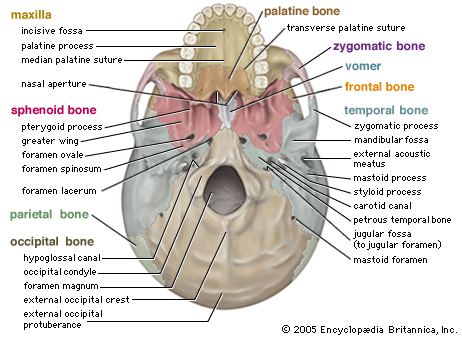
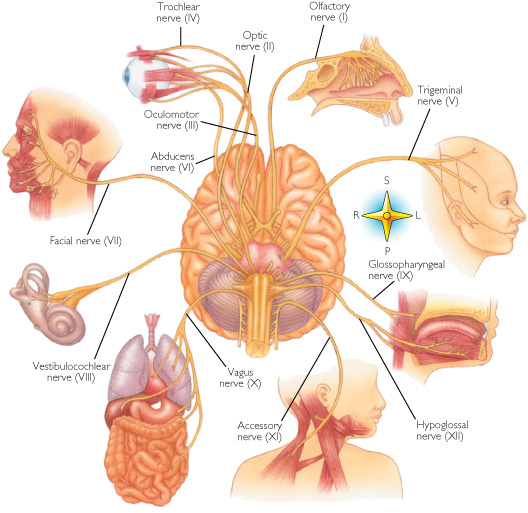
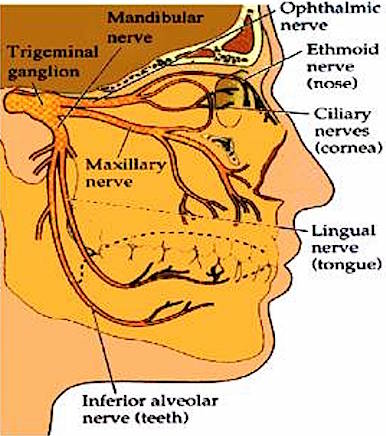
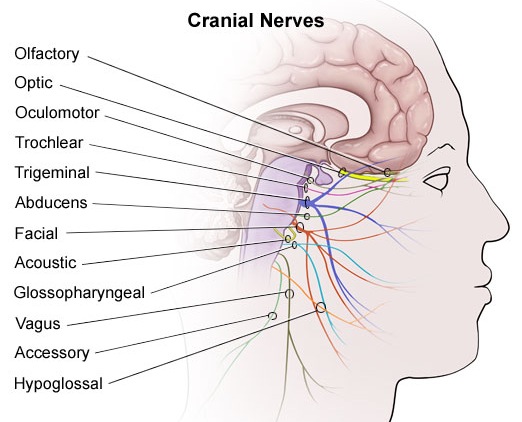
In some instances these fractures may extend in an anterior, posterior or lateral direction. If they extend in an antero-lateral direction, tearing of the olfactory, optic, oculomotor, trochlear, first and second branches of the trigeminal, and the facial and auditory nerves may occur, thus disrupting olfaction, vision, eye movements, and/or cause unilateral facial paralysis and hearing loss.
If extending laterally they may damage the mastoid bone and tympanic membrane of the inner ear resulting in dizziness and disturbances involving equilibrium. and a loss of hearing.
Basilar fractures are sometimes associated with tearing of the dura as well as CSF leakage. Hence, a variety of related complications may occur including infection.
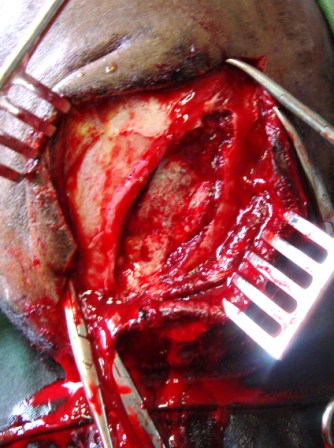
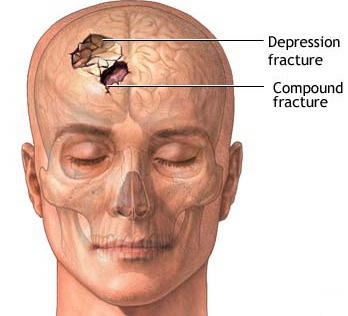
DEPRESSED FRACTURES
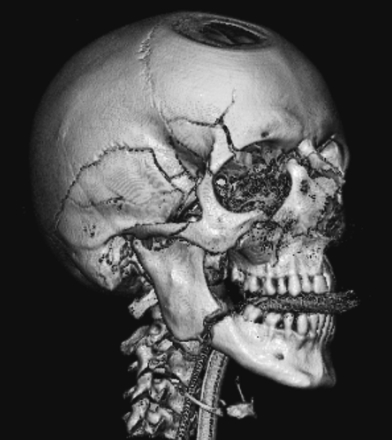
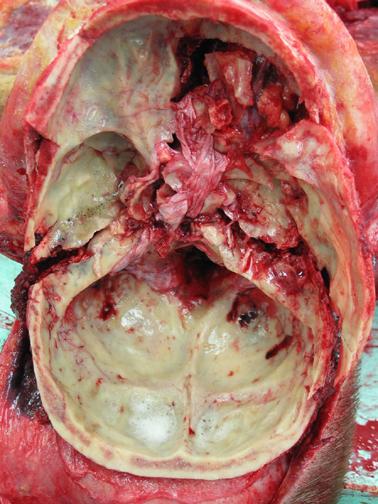
Usually with depressed fractures, part of the skull will shatter into several fragments which are driven downward toward the brain. The outer surface of the brain is covered by the dura and meninges, and the various compartments of the brain such as the cerebral hemispheres are separated by a tough leather-like material such as the falx cerebri.
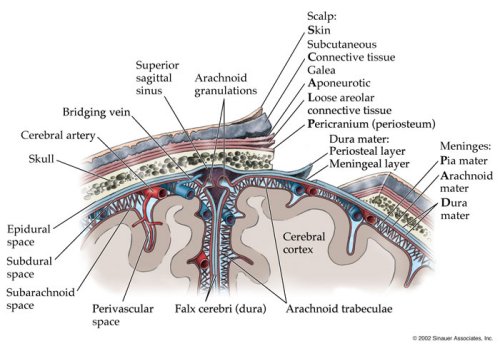
If the dura is torn the brain is often lacerated as well. Moreover, if the dura has been torn the patient becomes vulnerable to infection, particularly in that pieces of hair or other debri may be driven into the cranial vault. This in turn will later give rise to a host of symptoms including the possible development of meningitis (Jennett & Teasdale, 1981).

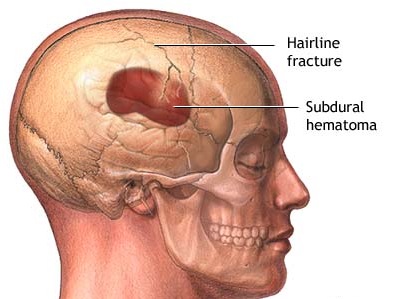
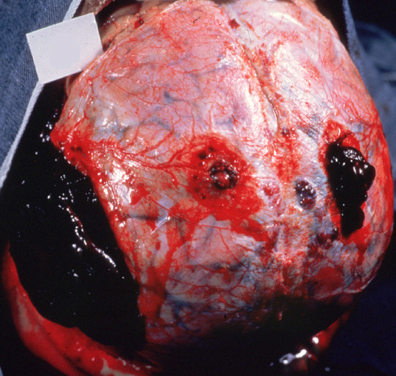
Frequently, but not always, the meningeal artery may be torn and intracerebral, extracerebral or an epidural hematomas may develop. Laceration and contusions are usually found beneath the broken bone fragments, and subdural hematomas may develop on the contralateral side (Bakay et al., 1980). If not accompanied by a laceration of the scalp, depressed fractures are described as closed.
In some cases, particularly if bone fragments have been driven into the brain and/or with the development of hematomas, patients develop focal neurological signs depending on which part of the brain has been compromised.
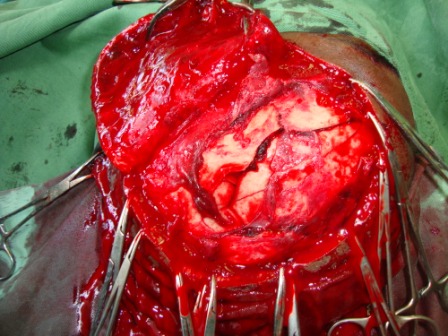
Approximately 50% of those who suffer a depressed skull fracture do not lose consciousness (Bakay et al., 1980; Jennett & Teasdale, 1981) and in many instances the dura is spared and there is no gross evidence of neurological compromise. This does not mean, however, that the brain has not been injured.
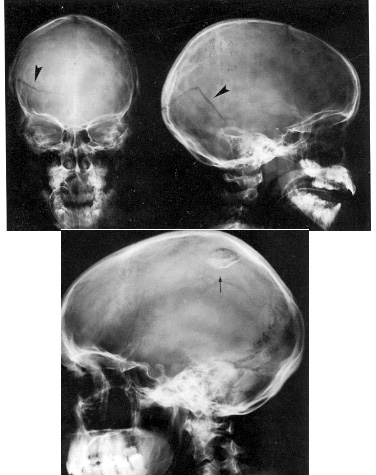
LINEAR FRACTURES
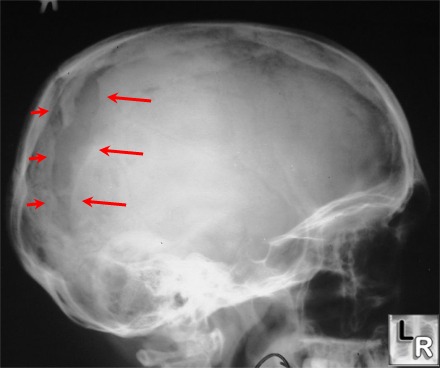
When the head is struck there usually results an inward deformation of the skull immediately beneath the site of impact whereas the surrounding area is bent outward. In some instances the skull shatters (i.e. depressed fracture) whereas in the majority of cases it will crack. Linear fractures are of two types, longitudinal and transverse.
Like depressed fractures, patients may or may not lose consciousness. However, it has been reported that patients with linear fractures who retain consciousness are 400 times more likely to develop a mass lesion (e.g. hematoma) as compared to comatose patients who are 20 times more likely to develop intracranial hemorrhage (Jennett & Teasdale, 1981).
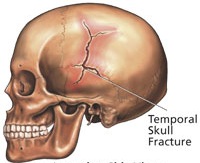
The most common sites of linear fractures involve the temporal and parietal bones. Indeed, the temporal portion of the skull may fracture following trauma to any portion of the cranium.
HEARING LOSS, VERTIGO, DIZZINESS, & BLINDNESS
Linear fractures involving the temporal-parietal bones may damage the auditory meatus, eustachian tube, and ear drum causing hearing loss, tinnitus, disorders of equilibrium and vertigo.
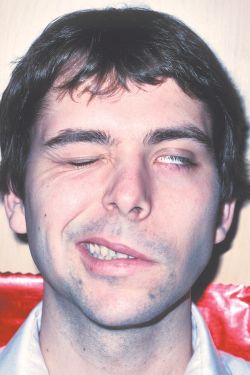
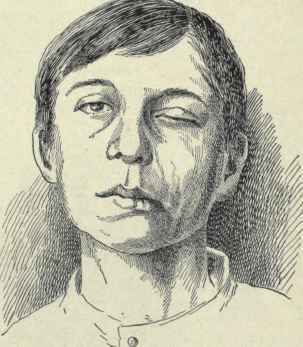
Facial Paralysis.
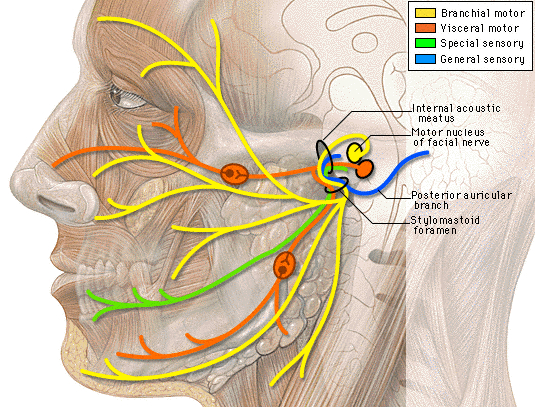
In some instances, longitudinal fractures may damage the cochlear nucleus and cause injuries to the 7th and 5th cranial nerves which pass through this area before innervating the skin and muscles of the face. When these nerves are crushed or damaged there results a unilateral facial paralysis and loss of sensation. Transverse fractures can also cause stretching of the 7th and 8th nerves and may damage the vestibular and cochlear portions of the labyrinth. Hence, facial paralysis and hearing related abnormalities may also occur.
Anosmia.
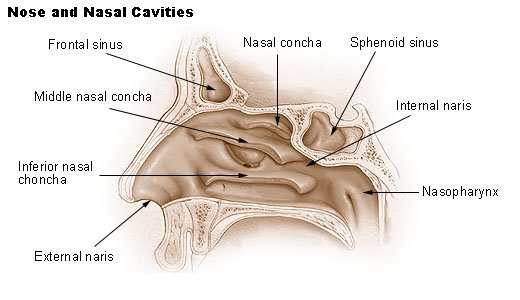
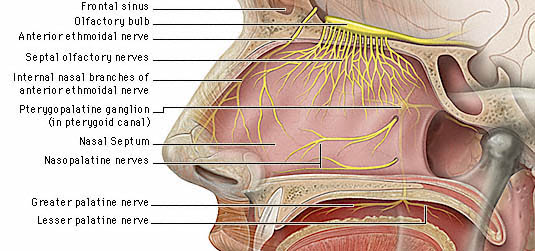
Anosmia (loss of the sense of smell) and an apparent loss of taste (loss of aromatic flavor perception) are frequent sequalae of head injury, especially following injuries to the face and fractures involving the back of the head or frontal bone. Anosmia is due to damage to the olfactory nerve, usually in the vicinity of the cribiform plate.
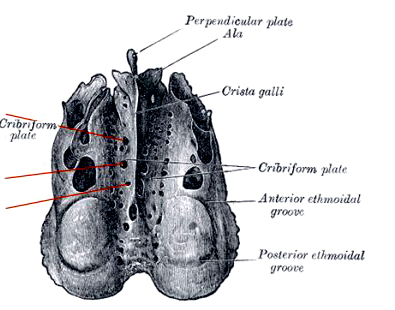
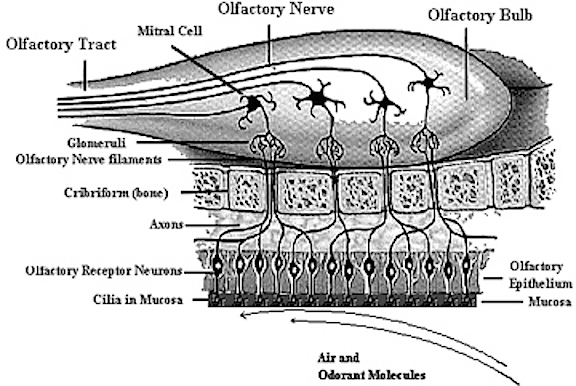
The cribiform plate is a wafer thin sheet of perforated bone through which the olfactory nerves pass on their journey from the nasal mucosa to the olfactory bulbs. Because this thin sheet of bone is perforated it is predisposed to fracture during head trauma regardless of where the patient was struck. This may cause the olfactory nerves to shear off thus resulting in a permanent loss of smell--anosmia. Patients are unable to even detect markedly unpleasant odors. If odors can be detected, the olfactory nerve is intact.
If the shearing is unilateral the loss of smell will not be recognized by the patient. It is only with complete bilateral shearing that patients begin to complain, usually noting that they have suffered a loss of taste.
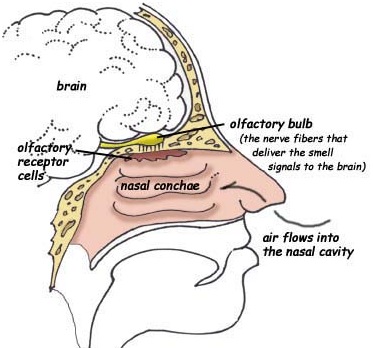
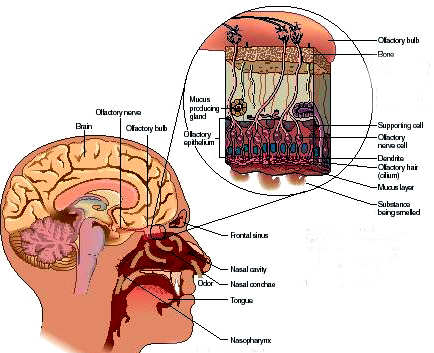
With damage to the olfactory nerve and cribiform plate, sometimes there also may result a laceration or rupture of the meninges, If there is meningeal rupture cerebrospinal fluid will leak into the nose. Frequently the only symptom is what appears to be a continually "running nose". In some instances cerebrospinal fluid has gushed into the patients nose when he has coughed or sneezed --well after the injury. Hence, if a patient has a runny nose, loss of smell, but no cold or allergy, and has had a head injury, a cerebrospinal fluid fistula secondary to meningeal rupture and cribiform plate fracture should be considered. If this is suspected he should be referred immediately to a neurosurgeon. Sometimes a secondary consequence of rupture which goes untreated is bacterial infection which may develop into meningitis.
Blindness.
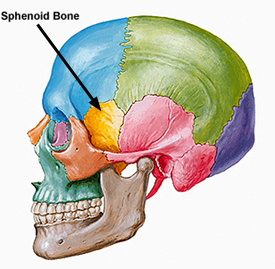
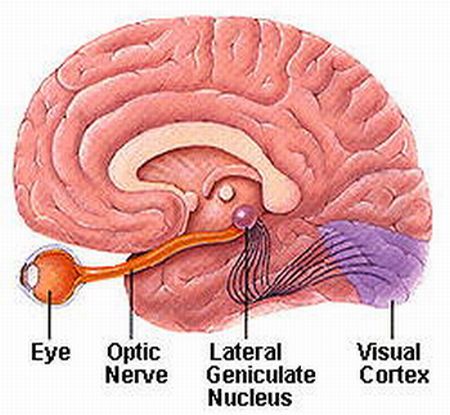
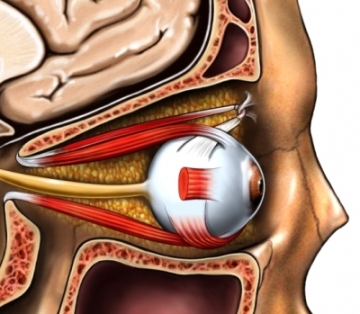
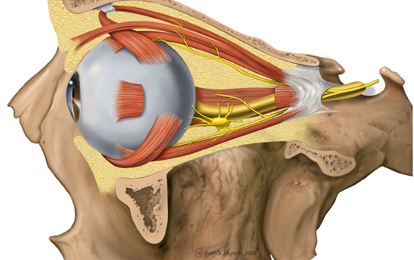
Fractures near the sphenoid bone (which juts out beneath and below the frontal bone within the skull) may result in laceration of the optic nerve. When this occurs the patient becomes immediately and permanently blind. The pupil becomes permanently dilated and is non-reactive to light, although consensual reflexes are maintained.

In some cases an individual may be struck so hard that their eyes pop out of their sockets. In others, although the eyes do not pop out, their main be strain on the optic nerves thus causing visual problems and light sensitivity.
Various definitions for what constitutes a "mild head" injury have been offered, many which differ in regard loss of consciousness, severity of injury, degree of memory loss, and so on (see Teasdale 2004, for related discussion). In consequence, the ability to accumulate reliable data on associated disturbances and recovery is therefore compromised. Moreover, as noted, many view mild head injuries as inconsequential when in fact that may not be the case (Kelly et al. 1991; Leininger et al. 1990; Miller 1993; Montgomery et al. 1991; Newton et al. 1992).

Moreover it is often erroneously assumed that consciousness must be lost in order for brain damage to occur. However, there is much evidence which indicates otherwise. In fact, as noted above, brain injury from shearing injuries (Adams et al. 1989), even in the absence of a head injury has been documented (Gennarelli 2006). In addition, what appears to be mild may be quite serious, even when CT scan and MRI fail to indicate brain damage (Newton et al. 1992). Indeed, some patients will die from a "mild" injury. On the other hand, the after-effects may also be quite insignificant.
In general, the period which encompasses "mild" for many investigators includes PTA and a loss of consciousness for up to 1 hour. However, even a loss of consciousness for less than 20 minutes can be quite serious, regardless of the extent of PTA.
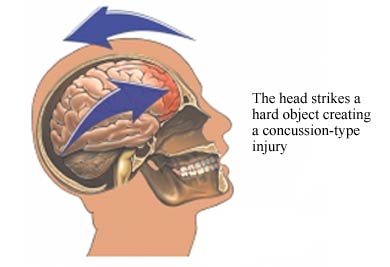
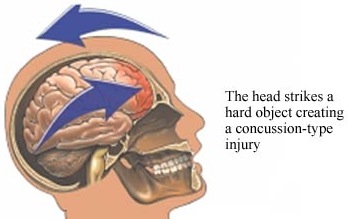
CONCUSSION
Although an individual may suffer a concussion and memory loss without losing consciousness, concussion is characterized by a brief period of unconsciousness followed by an immediate return of consciousness. There are usually no focal neurological signs and the loss of consciousness is usually due to mechanical forces such as the blow to the head. As the magnitude of the applied force is increased the severity of the concussion increases.
Often immediately after an insult to the head the patient will drop motionless to the ground and there may be an arrest of respiration and an eventual fall in blood pressure (following a rise at impact)--death can occur from respiratory arrest. Vital signs usually return--even if the patient is unconscious--within a few seconds. Once respiration returns, the patient may begin to move about in a restless random fashion and may speak, usually unintelligibly. They may become abusive, irritable, shout, and resist contact.
MILD & CLASSIC CONCUSSION
As described in detail by Gennarelli (2006) there are two broad categories of concussion as well as distinct subtypes. These include mild concussion in which there is no loss of consciousness, and classic concussion which involves a short period of coma.
MILD CONCUSSION.
Mild concussion consists of several subtypes, these include focal concussion which is due to involvement of a localized region of the cerebral cortex. For example transient left sided weakness may be due to right motor involvement, whereas the patient who sees "stars" may have received an occipital injury. A diffuse concussion results in transient confusion and disorientation. In either instance these concussive injuries may or may not be accompanied by amnesia.
With greater impact, although the patient does not lose consciousnesw they may be confused, disoriented, and continue to motorically interact with their environment (Kelly et al. 1991; Yarnell & Lynch, 1970). That is, they may walk around and even speak to others. However, although immediate recall is intact, they later become amnesic for the event as well as the events leading up to the injury; i.e. anterograde and retrograde amnesia. The anterograde and retrograde amnesia may extend forward and backward in time for up to 20 minutes even without loss of consciousness (Yarnell & Lynch, 1970). When this occurs it is evident that they have suffered a significant insult to the brain.
CLASSIC CONCUSSION.
Classic concussion is accompanied by a brief loss of consciousness at the instant of injury and is almost always associated with post traumatic amnesia. However, according to Gennarelli (2006), a patient with a classic concussion may remain unconscious for as long as 6 hours. If longer than six hours the patient has probably suffered diffuse axonal injuries such that large scale regions of the cerebrum have become partially disconnected.
In general, a mild (classic) concussion is associated with amnesia of less than one half hour, a moderate concussion with amensia of 1-24 hours, and severe concussion with amnesia of 24 hours or more. Nevertheless, although the concussion may be considered mild, the accompanying brain damage may be minimal, moderate, or in a few rare cases severe.
In cases of classic concussion, immediately following the injury the patient develops apnea, hypertension, bradycardia, cardiac arrhythmias, and neurological disturbances such as decerebrate posturing and pupillary dilation. Thus the patient may seem temporarily paralyzed. Often, upon regaining consciousness they will vomit and complain of headache. Even in mild cases, there can result temporary alterations in the permeability of the blood bain barrier, and damage involving the neuronal mitochondria.
MILD HEAD INJURY
A mild head injury is usually indicated by a GCS score of 13-15, no CT or radiological abnormalities, and a loss of consciousness for less than 20 minutes (some authors, however include those with unconsciousness lasting up to 1 hour, (e.g., Dikmen et al., 2006). This has also been referred to as cerebral concussion and patients need not have lost consciousness at the time of injury (Dikmen et al. 1983).
Although described as "mild" these injuries can be quite serious and involve various degrees of permanent brain damage. For example, anywhere from 1- 5% of those with mild head injuries may demonstrate focal neurological deficits (Coloban et al. 2006; Rimel et al., 1981). In addition, 2-3% of those with mild injuries deteriorate after initially appearing alert and responsive (Dacey et al., 2006; Fisher et al., 1981). Moreover, 3% of those with mild head injury will develop increased intracranial pressure and life-threatening hematomas which must be removed (Dacey et al. 2006). Indeed, approximately 1 out 100 individuals with mild head injury die (Luerssen et al., 1988).
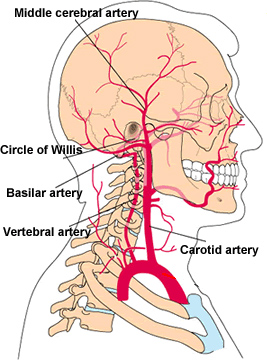
HYPOXIA & BLOOD FLOW
The energy required to run the brain is produced via the oxidative metabolism of glucose. Indeed, the brains need for these substances is quite substantial as it utilizes almost 20% of the bod's oxygen supply (which the brain is unable to store), and consumes over 25% of total body glucose. The source for both is the vascular system.
Reduction in oxygen and glucose create disturbances involving neuronal functioning, including dizziness, confusion, seizures and/or a temporary cessation of brain activity and coma--even if the deprivation is transient (Morgan & Gibson, 1991; Sokoloff, 1981). If prolonged the consequence is neuronal death. Reductions in the brain's oxygen supply is referred to as hypoxia.
In general, mild degrees of hypoxia are associated with dizziness, confusion, blurring of vision or difficulty seeing in the dark, whereas, moderate degrees produce loss of vision, nausea, coma and amnesia (Morgan & Gibson, 1991; Sokoloff, 1981). If prolonged there results severe permanent neuronal damage, coma and death. This is a serious concern as anywhere from 50-70% of those with severe head trauma are hypoxic following injury (Klauber et al., 1985). However, as neocortical oxygen and glucose uptake reaches its peak between the ages of 5-6 (Sokoloff, 1981), with consumption levels approaching 50% of all body oxygen, children can often be more severely effected by hypoxia.
Characterisically, following head trauma there is an immediate and global reduction in cardiac output and blood flow for a few seconds, which in turn results in oxygen deprivation. This is followed by a transient hypertension and then a prolonged hypotension (Crockard et al. 1982). The overall consequences are reductions in arterial blood perfusion and thus hypoxia throughout the brain as well as decreased blood flow within the damaged tissue. Metabolism is disrupted and energy failure occurs. In addition, the brains blood and oxygen supply can be reduced or diverted following chest injury, scalp laceration, or fractures involving the limbs.
Unfortunately a vicious deteriorative feedback cycle can be produced by these conditions which further reduces the brains supply of blood and oxygen. For example, hypoxia induces vasodilation and constriction of the blood vessels, a condition which results in intracranial hypertension. This creates an overall increase in intracranial pressure. When intracranial pressure increases the brain and blood vessels become compressed (due to displacement pressure) which further reduces blood and oxygen flow within the brain and to the damaged tissue. This causes the development of ischemia and focal cerebral edema (Jennett & Teasdale, 1981; Miller, 1985) all of which in turn add to displacement pressures (herniation).
RESPIRATORY DISTRESS.
With severe head injury many patients may also suffer from transient disturbances involving respiration and apnea (Miller, 1985); i.e. a decrease in respiratory rate. With decreased respiration there is decreased reoxygenation of the blood all of which favor the development of hypotension and hypoxia (Staller, 1987).
With respiratory distress, hypotension, and hypoxia, there results pulmonary hypoperfusion and an increase in blood platelets in the capillaries. Unfortunately, the increased number of blood platelets actually act to obstruct the blood vessels thus further reducing blood flow. This has been referred to as neurogenic pulmonary edema. Onset if often delayed and may occur 48 hours after injury. However, arterial hypotension may be an immediately sequela if there has been blood loss from a scalp laceration or other injury (Miller et al., 1981).
Vascular trauma.
Frequently, particularly with severe head injuries, the vasacular system may be traumatized due to shearing and stretching of the blood vessels. Moreover, the blow itself or the action of rotational forces can cause vascular spasms of the carotid arteries as well as the anterior and middle cerebral arteries (Bakay et al, 1980). Although vasopasm can temporarily increase cerebral blood flow, it also increases the likelihood of stroke and or blockage of the small arteries due to the breaking off of tiny plaques and other debri lining the large vessel walls (Chapter 33).
Myocardial trauma.
Head trauma can also result in secondary cardiovascular abnormalities including myocardial damage. For example, if the brainstem medulla has been compromised, there may be abnormal activation of the vagus nerve which influences heart rate, the result being atrial fibrillations--a condition which in turn sometimes results in stroke.
It is important to note, that even with a minor head injury, if there is an injury to the chest (i.e. a penumothorax, hemothorax), hypoxia may be produced due to inadequate ventilation of air. For example, due to pulmonary edema or lung shunting, the ability of the lungs to transport oxygen to the blood is reduced (systemic hypoxia). This results in brain damage even if cerebral blood circulation is normal.
Summary.
Hence, a variety of conditions associated with head injury can conspire to produce widespread hypoxia and disturbances involving cerebral metabolism. Neuronal death, independent of impact or rotational acceleration-deceleration forces is the long term consequence, even in mild cases. Hence, an individual with a minor head injury may suffer graver disturbances than an individual with a more serious injury if bones were broken or if the chest were injured.
Brainstem Abnormalities.
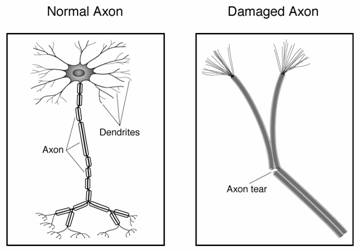
It has been suggested that sheer-strain secondary to mild acceleration-deceleration injuries cause tearing of axons which is followed by degeneration of the neural tracts in the brainstem. Brain stem axonal degeneration has been experimentally demonstrated in monkeys with mild acceleration-deceleration induced injuries (Jane et al.1982), and among humans up to 40% of those with "mild" head injuries may demonstrate abnormal brain stem evoked potentials (Montgomery et al. 1991; Rowe, & Carlson, 1980). Similarly, those who have died from other causes demonstrate, microscopic neuronal damage, micro glial scars and fiber degeneration within the brainstem and cerebral hemispheres --even among those who received what was considered "trivial" injuries (Oppenheimer, 1968; Strich, 1969).
DAI & Contusions.
Diffuse axonal injuries (DAI) have been noted among those suffering brief period of unconscious (Teasdale & Mendelow, 1980). Moreover, contusions within the anterior temporal regions and frontal lobes have been found among those with mild non-impact concussions due to acceleration/deceleration injuries (Adams et al., 1981).
NEUROPSYCHOLOGICAL DEFICITS.
Individuals with mild head injuries have been repeatedly shown to suffer a variety of neuropsychological, psychosocial, and emotional impairments even in the absence of gross or focal neurological deficits. These include pervasive neurobehavioral impairments involving attention, memory, and rate of information processing. Patients may suffer word finding and expressive speech difficulties, reduced reaction time, perceptual-spatial disorders, and abnormalities involving abstract reasoning abilities. Moreover, although generalized recovery is often noted within 3 months of injury, a memory disturbances often remains and may in fact persist for years.
In some studies it has been reported that at 3 months post mild injury a significant number of individuals continue to demonstrate visual spatial abnormalities, memory disorders, reduced ability to concentrate, and persistent headaches, and as many as 34% of those with mild injuries may be unemployed at this time (Barth et al. 1983; Rimel et al., 1981). Interestingly, these deficits are not in any manner correleated with length of unconscious or PTA, and in one study only 6 of over 400 patients were involved in litigation. Hence, purposeful malingering is not likely among the majority of such cases.
PREMORIBID INFLUENCES.
It is noteworthy that recovery appears to be dependent on previous mental abilities (Dikmen & Reitan, 1976; Miller 1993) such that the debilitating effects of mild head injury appear to effect indviduals with minimal educational backgrounds more so than those with initially higher levels of functioning and education (Deb et al., 2012). This may be because these individuals have "bad brains" to begin with, and/or are less able to compensate for cognitive disturbances secondary to brain injury because of their more limited capabilities. That is, those with higher level abilities have more to draw from and to fall back on. Of course, they also have more to lose.
Following a mild (vs. severe or moderate) trauma to the head, patients may not begin to complain of cognitive disturbances until days or even weeks have passed (Alves et al. 2006; Miller 1993) even when consciousness has not been lost. Symptoms are often non-specific and are hard to quantify or objectively document. In general, these are referred to as post concussive disorders. Indeed, about 50% of those who suffer mild head injuries are at risk for developing post concussion symptoms (PCS). PCS is manifested somewhat different for adults vs. children.
Among adults, complaints regarding PCS may include persistent headaches, transient dizziness, nausea, impaired memory and attention, irritability, depression, anxiety, easy fatigueability, nystagmus, as well as inner ear disturbances such as vertigo, tinnitus, and hearing loss. Headache, dizziness, memory problems, weakness, nausea, and tinnitus are often the most common complaints--even at 12 months following injury (Alves et al., 2006; Zasler, 2012).
Other symptoms may include hyperacoutism, photophobia, decreased judgement, loss of libido, and difficulty with self-restraint and inhibition.
In contrast, children often may become withdrawn, antisocial, aggressive, develop enuresis, as well as sleep disturbances. Moreover, it has also been reported that some individuals, children in particular, develop transient migraine-like attacks following even minimal injuries where consciousness was not necessarily lost (Haas & Lourie, 1988). These attacks include blurred, tunnel, and/or partial or complete loss of vision, paresthesias, dysphasia, confusion, agitation, headache, drowsiness, and vomiting --all of which come on like spells, particularly soon after the injury. It has been suggested that this is due to traumatic spasm of the larger cerebral arteries.
In general, post-concussion symptoms are varied in their degree and duration, although frequently they may persists for long time periods, from months to year or sometimes indefinitely (Dikmen & Reitan, 1976; Merskey & Woodforde, 1972; Miller 1993; Symonds, 1962). Nevertheless, even when PCS begins to wane it is sometimes followed by a long period of depression.
EMOTIONAL SEQUELA.
Many patients with PCS in fact develop a variety of emotional and personality difficulties which seem to be triggered by the experience of having had an injury (Bennett, 1969; Deb et al., 2012; Miller 1993). Patients may seem extremely anxious, fearful, depressed, and/or preoccupied with the details surrounding the accident, and remain (albeit periodically and transiently) upset for long time periods . Others may appear intolerant of noise, emotional excitement and crowds, and complain of tenseness, restlessness, inability to concentrate, and feelings of nervousness and fatigue. That is, they demonstrate the signs of post traumatic stress disorder. Many patients with this syndrome also seem unable to tolerate the effects of alcohol. The emotional disturbances may persist for months or years, but usually lessens as time passes.
It has been argued, and frequently it is suspected that PCS has in fact no objective basis and represents an exacerbation of pre-morbid personality characteristics or is motivated by a desire for financial compensation (Miller, 1961). Undoubtedly this is true in some cases. Nevertheless, frequently the majority of such individuals are not even involved in litigation (Barth et al., 1983; Merskey & Woodforde, 1972; Rimel et al., 1981). Moreover, sometimes the actual deficit is greater than the patient realizes (Prigatono et al. 1990; Waddell & Gronwall, 2004).
Cerebral Blood Flow.
Neuronal damage involving the brainstem and cerebral hemispheres as well as significant decrease in cerebral blood flow have been demonstrated among patients with mild and trivial head injuries (Montgomery et al, 1991; Taylor & Bell, 1966). In fact, many of these same patients were without PCS complaints and demonstrated normal circulation during the first 12 hours after their injuries and then within a period of 3 days developed post concussive symptoms and decreased cerebral blood circulation which lasted weeks and months. It has been suggested that this may be secondary to vasomotor abnormalities due to brainstem (medullary) impairment (Taylor & Bell, 1966).
Attention & Information Processing.
It has also been shown that patients with PCS and mild head injury are unable to process information at a normal rate (Gronwall & Writhson, 1974) and tend to become over welmed. Frequently, however, patients do not complain about this until days or weeks later as this does not become apparent to them until they return to work and thus discover they are having problems. As such they may find that tasks which require attention to a number of details and which formerly were performed quite easily, now seem difficult and beyond their capacity. Hence, the patient says he cannot concentrate (Gronwall & Writhson, 1974; Miller 1993).
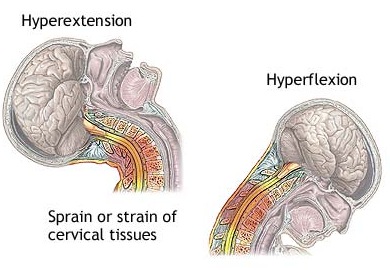
Presumably, many of the post-concussion symptoms are secondary to shearing forces associated with the acceleration/deceleration nature of their injuries as well as torque and other forces exerted on the brainstem. Indeed, following whiplash, patients may develop PCS, including vestibular symptoms and dizziness.
Whiplash & Blood Flow.
In whiplash the head is like a ball at the end of a whip and rapid or extreme rotations or extensions of the head may cause decreased blood flow by compressing the veterbral arteries which supply the brainstem, cerebellum, occipital lobe and hippocampal region of the temporal lobe (Chapter 33). This leads to symptomatic vestibular insufficiency and other brainstem responses (feelings of giddiness, lightheadness, loss of balance), and can exert disrupting effects on memory and visual functioning. If the patient is suffering from atherosclerosis or abnormalities involving the cervical vertebrae (e.g. cerical osteoarthritis) the overall effects can become exacerbated even further.
Similarly, as is well known, the internal carotid artery is also very vulnerable to trauma, particularly in the neck where it is exposed. Hence, rapid extensions and rotations as well as karate-like blows, can tear and dissect the artery resulting in obstruction.
In general, tall persons suffer whiplash more often than shorter individuals, and those riding in the front of an auto are 50% more likely than those in the rear of sustaining such an injury (Elia, 1972). Slow speed crashes carry a greater chance of whiplash injury than high speed due presumably to patients becoming tense in realization of the impending accident.
As noted, acceleration/deceleration injuries are most likely to effect the brainstem, temporal and frontal lobe. In fact there is some suggestion that frontal injuries are more likely to give rise to postconcussional disturbances (Rabavilas & Scarpalezos, 1981). However, brainstem and temporal lobe abnormalities are obviously contributory.
Vertigo, Hearing Loss & Tinnitus.
Damage to the inner ear (which is situated within the temporal bone) is frequently associated with the development of vertigo, dizziness, and tinnitus. As noted, the temporal bone (which contains the auditory meatus) is often subject to injury, including fracture regardless of where the head was initially struck. Hence, the presence of vertigo and tinnitus following a head injury suggest a concussion of the ear ear (Elia, 1972).
Some patients also complain of hearing loss or even unilateral deafness. In some cases this is secondary to an injury of the tympanic membrane, external auditory canal, or the inner skin of the ear. This results in some bleeding and thus the potential development of dried blood clots (and cerumen) in the auditory canal which subsequently plug the ear reducing auditory acuity by impeding sound transmission. In addition, in cases of temporal bone fracture, cerebrospinal fluid may escape into the ear thus temporarily disrupting functioning.
On the other hand, some patients complain of increased sound sensitivity. It has been proposed that this is secondary to rotational acceleration forces which stretch and cause traction of the stapedius muscle which is attached to the vestibule and stapes of the ear.
Diploplia & Photophobia.
It has been proposed that visual problems such as diplopia may occur secondary to traction of the eye muscles. That is, the eyes may almost pop out of the socket, or they may actually pop out of the socket, which of course would put considerable strain on the optic nerve. If the oculomotor nerve is injured in any manner, this too may cause diplopia and may also contribute to the development of nystagmus (Elia, 1972). Nystagmus usually resolves over time.
Photophobia and excessive sensitivity to light may also be secondary to oculomotor traction. It has been demonstrated that many such patients with minor head injury are consequently more sensitive than they realize (Waddell & Gronwall, 2004), and some demonstrate a hypersensitivity to both sound and light when in fact this was not a complaint.
PCS & Severe Head Injury.
It has been noted that those with mild injuries sometimes complain of PCS more so than those with severe injuries (Levin et al., 1987). This in turn has led to the unfounded suspicion that these disturbances have no objective basis. However, in some cases as patients recover and progress from severe to moderate or moderate to mild degrees of disability, they begin to make these same complaints. Moreover, there is some possibility that due to the greater degree of cognitive and personality disorganization among those with severe injuries that their ability to appreciate and complain of these disturbances is lessened (i.e. lack of insight, decreased motivation). In this regard, frequently patients with severe brain injuries do not become or demonstrate depression until after there has been considerable recovery (Merskey & Woodforde, 1972).
Individuals who sustain repeated head injuries sometimes have a history of emotional, impulse, and educational difficulties. Some individuals suffer head injuries because of reduced functional capabilities and thus place themselves in dangerous situations, drive recklessly, and so on. In fact it has been reported that as many as 50% of head injured indivduals have a history of poor premorbid academic performance, including learning disabiities, school drop out, multiple failed subjects, as well as social difficulties (Fahy et al. 1967; Fuld & Isher, 1977; Haas et al. 1987; Miller 1993).
The finding that many head, and even spinal injured patients (Morris, Roth & Davidoff, 2006) have also suffered previous cerebral traumas has led some investigators to suggest that these individuals have a life style which seems to predispose them to violence and injuries to the cranium (Tobis et al., 1982). As suggested by Haas et al., (1987), this relationship may be due to poor attention span, distractibility, limited frustation tolerance, poor judgement, impulsivity, difficulty anticipating consequences, perceptual-motor abnormalities, etc. all of which makes these individuals more susceptible for being involved in an auto accident. However, it is also possible that once someone has a head injury, due to subsequent decreases in overall functional efficiency, that they are less likely to avoid situations where a second (or third) injury may occur.
Life style and premorbid social-emotional stability are in fact important contributors to the possibility of suffering a head trauma. For example, chronic alcoholics are especially prone to cerebral injury (Bennett, 1969; Miller 1993). It has also been reported many head injured patients have suffered a bout of depression or other emotional disturbances (e.g. fight with a girlfriend) immediately prior to their injury (Tobis et al. 1982).
Overall, the individuals most at risk for suffering a head injury at some point in time are young males (Teasdale 2004), particularly those with a history of learning disability, alcohol abuse, social-emotional difficulties, and previous head trauma. Indeed, males are twice as likely to suffer head injuries as females and also more likely than females to engage in "risky" and "macho" behaviors, which of course puts them at the greatest risk. Conversely, it is also males who are more likely to downplay the significance of their injury and who will display the most resistance to rehabilitation, and in particular, psychotherapy.
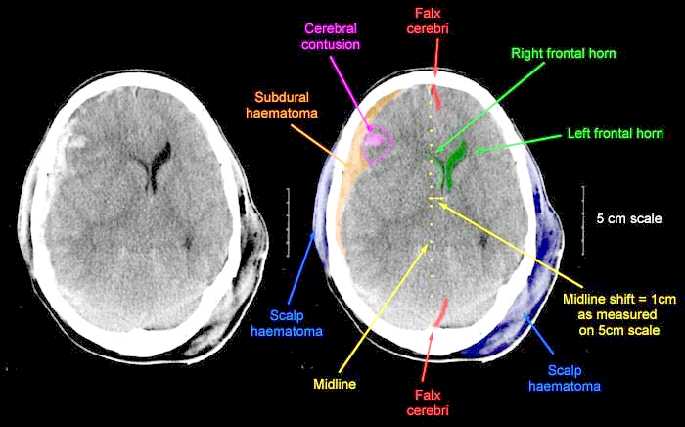
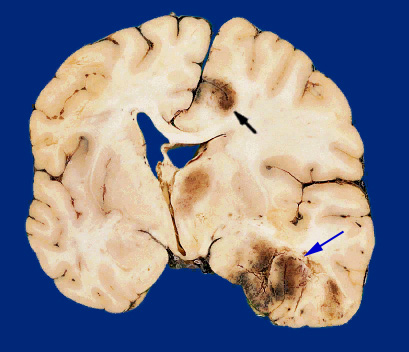
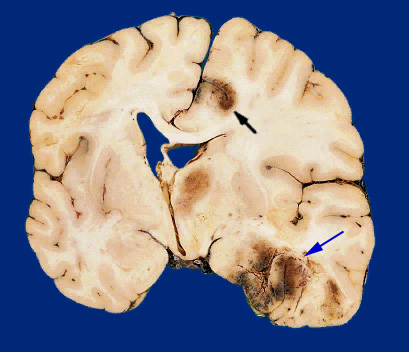
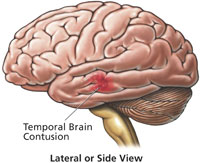
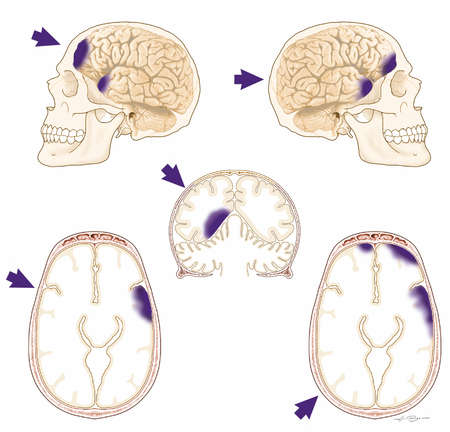
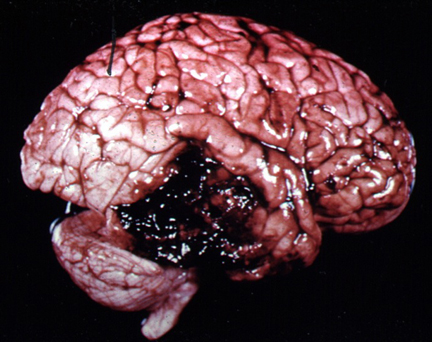
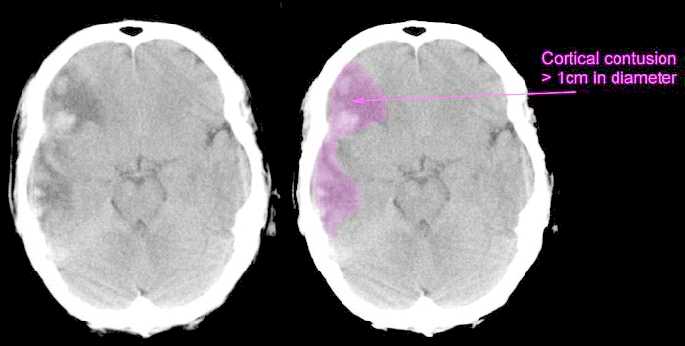
Usually the force of the impact will force the brain to shift, and/or bounce against and strike the inner bony prominences of the opposite half of the skull (i.e. contre coup injury) as well as the falx cerebri and tentorium (Leestma 1991). This results in contusions to the neocortical surface, particularly along the temporal and frontal lobes.
Contusions and bruises are usually found in the orbital frontal regions and anterior and lateral temporal lobes bilaterally as well as along the convexity regardless of where the skull was struck (Adams et al., 1980). Frequently the medial portions of the brain including the corpus callosum may also be traumatized due to rotational forces such that they bump and slide against the falx and/or tentorium. In contrast, contusions are rarely encountered along the occipital lobe, even when the back of the head has been struck.
In general, contusion may consist of multliple hemorrhages which develop immediately upon impact along the crests of the various cerebral gyri. Contusional hemorrhages may increase in size during the first few hours after injury, extending from the superficial layers of the neocortex into the white matter. Edema is usually a secondary consequence. Thus, widespread damage, varying in severity, is a likely consequence of head injury.
Necrosis.
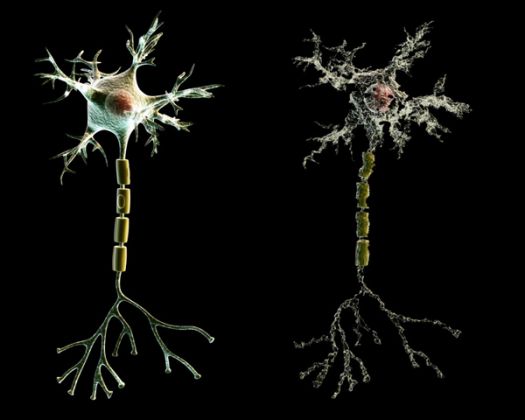
When the brain has been contused, severely compressed, or subjected to rotational shearing forces, axons are often severed and cells crushed. This results in cell death (necrosis) within the first 24 hours after injury --a process which may continue for up to a week. After a few months time these cells are reabsorbed leaving behind glia scars and small cavities in the cortex and white matter. These scars can in turn becomes a source of abnormal activity and may cause the development of seizures.
Axonal Transport Deficits.
Trauma to the brain may interfere in axonal transport in otherwise normal neurons (see Burke et al. 1992). When this occurs there may be a buildup of neurotoxics which in turn result in cell death throughout the neuroaxis. That is, if the post-synaptic neuron is injured, axonal transport to the damaged cell may become abnormal, such that in addition to a buildup of neurotoxicity, therby giving rise to neurofibrillary tangles, amyloid plaques, and cell death.
Consciousness.
When consciousness is not lost following a head injury it is frequently erroneously assumed that the brain was not damaged. However, a patient may in fact suffer significant cognitive disturbances and extensive contusions and lacerations throughout the brain even with no loss of consciousness. Moreover, there may be complete memory for the accident with no anterograde or retrograde amnesia.
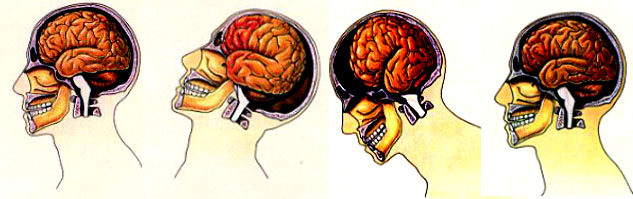
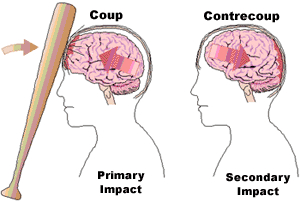
COUP & CONTRE COUP CONTUSIONS
In some instances it has been postulated that because of the differential movement of the brain there can result both coup and/or contre coup lesions. Coup contusions are due to the slapping effect of the skull hitting the brain. Tissue is damaged directly below the point of impact. Generally the head is stationary at the time of the injury.
Contre coup contusions are usually associated with translational linear acceleration injuries and the free movement of the head. Translational (linear) acceleration of the brain occurs at the moment of impact and/or as there is a rapid linear acceleration in the motion of the head --such as if thrown from a car. This causes the brain to bounce against and strike the rough bony protrusions on the opposite side of the skull.
Contre cavitation.
As pertaining to coup and contre coup lesions, rapid increases in acceleration sometimes cause the development of increased intracranial pressure at the trauma point, and decreased (contre coup) pressure at the opposite side of the cerebrum. In addition to the brain striking the opposite side of the skull, this decreased pressure at the contre coup site can cause the development of cavitation bubbles which, when they burst or collapse, cause local tissue damage, i.e. a contre coup lesion (Bakay et al. 1980). Contusions are often associated with this type of injury (Leestma 1991; Unterharnscheidt, & Sellier, 1966).
Differential effects of impact site.
The development of coup and/or contre coupe lesions are also dependent on what part of the skull was initially impacted. That is, impact to certain regions of the skull seem to commonly result in coup lesion, whereas other zones when struck give rise to coup and contre coup damage (Leestma 1991). For example, impact at the occipital region often forces the brain to move in an anterior direction causing a contre coup lesion to the frontal lobe (Bakay et al., 1980; Lindgren, 1966). Indeed, although there is some evidence of considerable movement of the parietal-occipital region regardless of the impact site (see Bakay, Glasauner & Alker, 1980; for review), direct blows to the occiput seldom cause occipital damage.
In contrast, impact to the front of the skull almost always results in frontal lobe (coup) injuries. However, in about 50% of the cases, both coup and contre coup lesions result. Temporal impacts also create contre coup lesions. If struck from the top of the head contre coup contusions frequently develop in the corpus callosum and the orbital frontal lobes due to the downward force of the blow (Bakay et al., 1980).
Caveats.
Not all investigators accept the notion of contra coupe damage, however. Indeed, the fact that the frontal and temporal regions are most severely effected regardless of, as does the findings that when there is a skull fracture, contusion are maximal on the side of impact. Rather, it has been postulated that much of the damage which occurs secondary to impact or non-impact (including coup and contre coup) injuries are due to the effects of rotational acceleration and shearing forces.
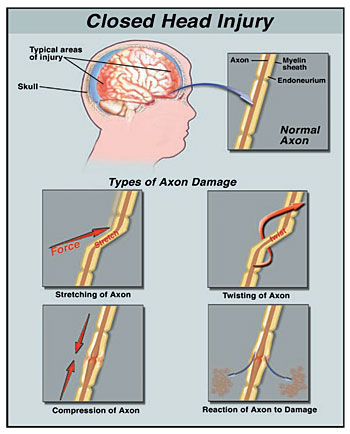
ROTATION & SHEARING FORCES
In certain types of head injuries, such as those involving a great deal of force and movement the brain will swirl, rotate, oscillate, and slosh around inside the skull in a rotary fashion. This can occur at the moment of impact or if the head is suddenly subject to rapid changes in motion (such as when the patient is air borne after been thrown through the windshield of their car vs. a blow to to the head when stationary). Indeed, rotational damage may occur even when the head has not been struck but can result from rapid skull movement alone, e.g. whiplash, severe and repeated shaking, or extreme motion of the head and neck (Adams et al. 1089; Uterharnschidt & Sellier, 1966). This is in contrast to linear acceleration injuries which are not usually associated with this differential swirling movement of the brain.
Nevertheless, as the brain swirls about the neocortical surface becomes contused, sliced and sheared by the the bony protrusions (e.g. the sphenoid wing) within the cranium and hemorrhages will develop over the surface of the cerebrum. The frontal-temporal regions are at particular risk for these type of injuries.
Brainstem & Subcortical Lesions.
However, rotational acceleration and decelerations injuries can create extensive subcortical and brainstem damage as well. For example, the cerebral hemispheres, brainstem and different parts of the brain will actually move in somewhat different directions as well as at different speeds thus inducing widespread stretching, straining and snapping of axons running throughout the white matter including the corpus callosum. Indeed, because these strains are not uniform but effect various parts of the cerebrum differently, such that one part of the brain is moving in one direction whereas another portion is sliding at a somewhat different angle, certain regions can literaly snap and break loose.
For example, when subject to severe rotational forces there sometimes is tearing at the pontine-medullary junctions (where the brainstem meets the midbrain), such that in consequence the brainstem is partly torn loose and disconnected from the rest of the brain (Hardman, 1979; Jennett & Plum, 1972). Because the cerebral hemispheres sit atop the thin brainstem, there can result torque in the pontine-midbrain junction thus disconnecting these lower from higher regions. When this occurs consciousness is lost and the patient either dies or remains in a prolonged coma.
In addition to contusions, rotational injuries are associated with venous tears, arterial shearing stresses, and hemorrhagic lesions in the midline region and throughout the brain. Nevertheless, the degree and type of damage which occurs is dependent on the speed, and direction at which the head moves. However, even presumably mild head injuries can induce brainstem injury.
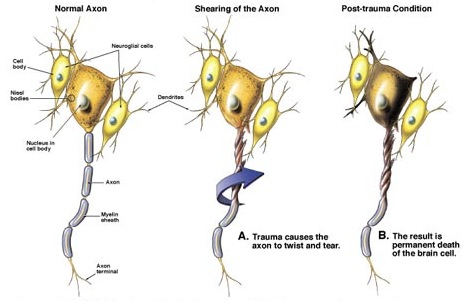
DIFFUSE AXONAL INJURY
Independent of actual impact, when the brain is subject to severe rotational and acceleration/deceleration forces, there can result severe diffuse microscopic damage and profound shearing and stretching of axons throughout the brain and brain stem as well as focal lesions in the corpus callosum. Axons are literally torn in half due to the twisting strains placed upon them. This condition is referred to as "diffuse axonal injury" (DAI).
When axons are severed or stretched the capacity to transmit electrical-chemical impulses and thus transmit information is attenuated. If severe, there can result a permanent loss of functional capability accompanied by an immediate and prolonged loss of consciousness. However, even in less severe head injuries subtle axonal injuries may result, including axonal swelling and impaired axonal transport and transmission (Povlishock 1992).
Conditions which give rise to DAI are also associated with brainstem damage, and decorticate and/or decerebrate posturing. When this occurs, many patients, if they survive, end up in a vegetative state. Most will die, however. If less severe there may be a temporary inability to function due to strains involving the axonal membrane (Adams et al. 1989; Gennarelli, 2006).
In general, DAI takes the form of axonal retraction balls in those who die within days, microglial scars in those who live days to weeks, as well as degeneration of the fiber tracts among those who survive for longer time periods, e.g. months. That is, a few days after an injury in which axons and nerve fibers have been torn, the nerve cell often dies and the glial cellular reactions around these damaged, dying, and dead cells, creates microglia scars. Often these scars can become epileptogenic.
Moreover, because of this diffuse damage, various and widespread regions of the brain are no longer able to function or intercommunicate; i.e. disconnection. Because of this, patients with DAI who have lost consciousness yet continue to live tend not to regain consciousness but remain in a prolonged coma. Interestingly, This condition occurs more frequently among individuals who do not suffer skull fractures.
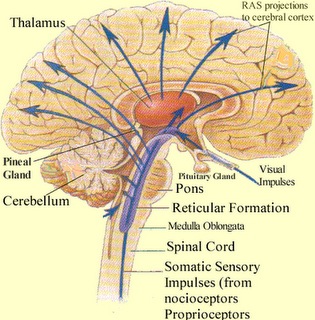
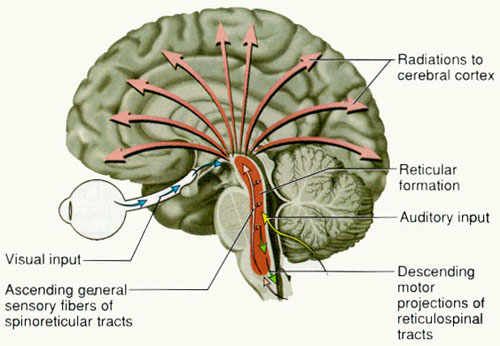
Consciousness may be lost following even "minor" head injuries. Likewise, with a "minor" head injury, patients may slip into a coma. If loss of consciousness and the development of a prolonged coma is immediate, it is likely that the brainstem has been injured. If consciousness is lost and the coma develops minutes or hours after the head injury, the cause is likely due to intra-cerebral bleeding and compression of the brainstem as the cerebrum is squeezed (by the developing pool of blood) into the formen magnum (at the base of the skull), thus injuring the brainstem--the brainstem mediating not only consciousness (via the reticular formation) but vital functions such as heart rate, breathing, and so on.
RETICULAR DAMAGE & IMMEDIATE LOSS OF CONSCIOUSNESS. In general, it is believed that the loss of consciousness following a brain injury is often due to abnormalities involving the reticular activating system of the brainstem.
Destruction of the brainstem reticular formation invariably induces states of prolonged unconsciousness and unresponsiveness, which is accompanied by a slow, synchronized EEG, and frequently irreversible coma; i.e. the remainder of the brain cannot be activated. However, damage need not be severe or extensive for even small lesions in the brainstem, midbrain and thalamus can induce a protracted loss of consciousness.
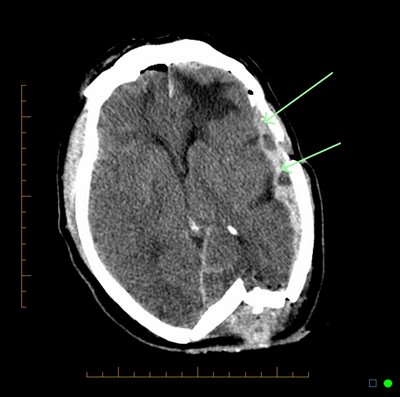
HEMATOMAS & HEMMORHAGE
Frequently brainstem, midbrain, and thalamic damage are secondary to acceleration rotational forces. These brain structures may also be damaged as a consequence of intracranial hemorrhage, ischemia, compression and herniation. However, these effects of trauma may also be slow to develop. That is, a small artery or capillary may be damage resulting in a slow and gradual loss of blood (e.g. epidural hemorrhage), in which case patients will lose consciousness sometime after the injury. These conditions are also associated with temporal-parietal fractures and laceration of the middle meningeal artery and vein.
Nevertheless, in these later instances the patient may seem normal for some time after the accident. However, as blood continues to leak and the brain becomes increasingly compressed, within a few hours or even days the patient begins to complain of headache, drowsiness, and confusion. With increasing blood loss the patient may suddenly experience seizures, hemiparesis and eventually loss of consciousness. If blood loss continues there is a great threat of temporal lobe herniation and eventual crushing of the midbrain. Hence, these disturbances are life-threatening and requires surgical intervention and identification of the bleeding vessel.
Loss of consciousness sometime after the injury is not always due to the development of hemorrhage. In some instances pain and emotional upset give rise to a vasopressor syncopal attack. Thus, following the injury the patient may walk about the room, seemingly returning to normal, and then turn pale and fall unconscious to the ground. In contrast, those who develop a hemorrhage or other disturbance lose consciousness at the time of injury but regain it after a few moments or minutes, only to fall back into unconsciousness later.
HEMOTOMAS
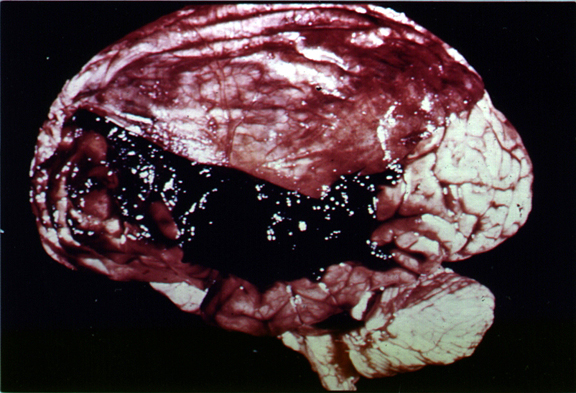
Following a head injury, with or without skull fracture, the arteries and veins running above, below, or through the meningeal membranes (which cover the brain) may be stretched, broken, pierced, or ruptured. This results in blood loss and the development of a a blood clot, a hematoma.
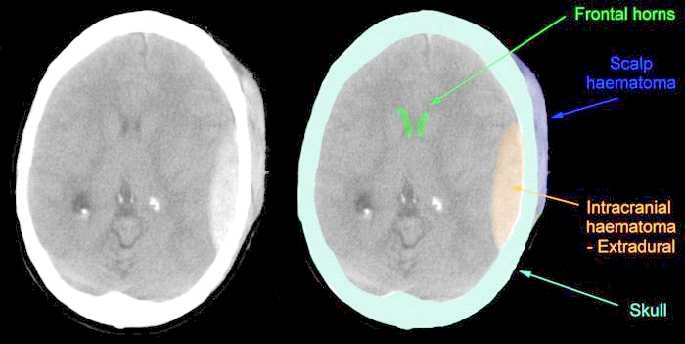
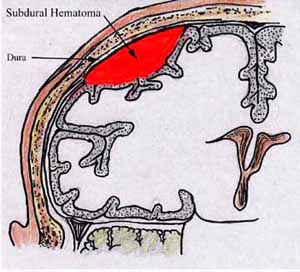
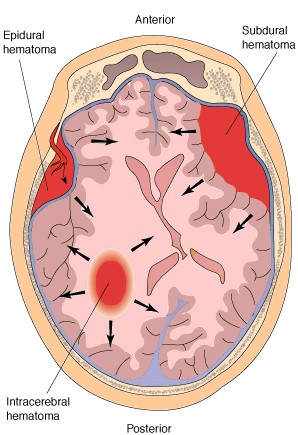
There are various types of hemotomas. Some form below the dura, i.e. intradural hemotoma, whereas others develop between the skull and the meninges and are referred to as extradural.
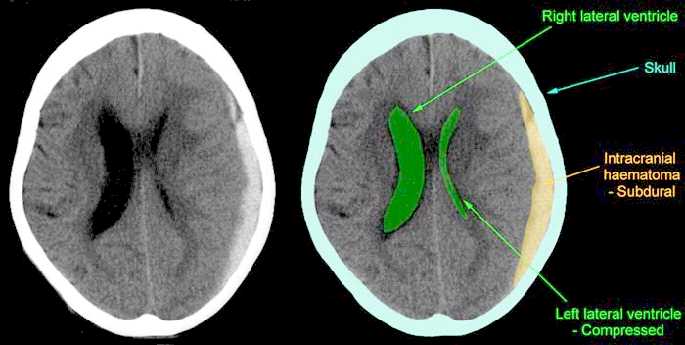
INTRADURAL HEMATOMAS
There are several subtypes of intradural hemotoma, i.e. epidural, subdural, intracerebral all of which may occur and develop immediately at the time of primary insult, or slowly thus causing symptoms days, weeks or even months after the original head injury. Although 30-55% of those with severe head injuries develop hematomas, they also occur with mild injuries.
Intracerebral hematomas are not very common. They are usually secondary to ruptured aneurysms, gunshot or stab wonds, and lacerations from depressed skull fractures.
Epidural hematomas are also not very common as they tend to occur in less than 10% of all patients with severe head injury. Most are secondary to fractures of the temporal-parietal area and laceration of the middle meningeal artery. They are frequently quite slow to develop, appearing hours or even days after the injury.
In most cases a patient will be struck and lose consciousness for a brief time period. Upon waking they seem lucid, but then as the hematoma develops they begin to increasingly complain of headache, irritability, confusion. As the hematoma increases in size and compresses and damages the brain the patients symptoms become more severe and consciousness may again be lost. If the hematoma is not evacuated the patient is likely to die (Gallagher & Browder, 1968).
Subdural hematomas are the most common of all and are associated with a very poor prognosis. These hematomas develop following damage to the various veins criss-crossing the subdural space. This results in a pool of blood developing over the surface of the entire brain. Patients may slowly or rapidly deteriorate and become markedly depressed or even stuporous as the hematoma enlarges and increasingly compresses the brain. In slowly developing undetected cases patients may continually complain of headache, develop alterations in personality as well as changes in level of consciousness. Eventually they may develop hemiparesis, language disorders, and other focal signs. Mortality has ranged from 30-70%--even when removal of the hematoma is attempted (Nikas, 1987).
Unfortunately, CT-scan (Cooper et al., 1979), and in particular, MRI (Snow, Zimmerman, Gandy, et al., 2006), are not very useful in detecting the initial development of subdural hematomas, even when associated with hemorrhage (see Newton et al 1992, for related discussion). Hence, although an initial CT-scan may have been normal, if a patient subsequently deteriorates, the possibility of hematoma should be entertained.
Chronic Hematomas.
Acute and chronic subdural hematoma may be unilateral or bilateral with an onset latency period of days or weeks. There may be headache, drowsiness, confusion, and disturbances in consciousness, all of which progressively worsen. Focal or lateralizing signs are less prominent. In the chronic condition, the traumatic etiology may not be clear or may seem very minor (e.g., striking the head against branch of a tree), particularly among older individuals. Headaches, giddiness, slowness in thinking, may not develop until weeks after the initial injury and may give the initial impression of a vascular lesion, tumor, or drug intoxication.
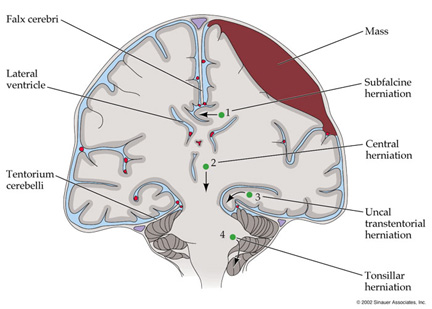
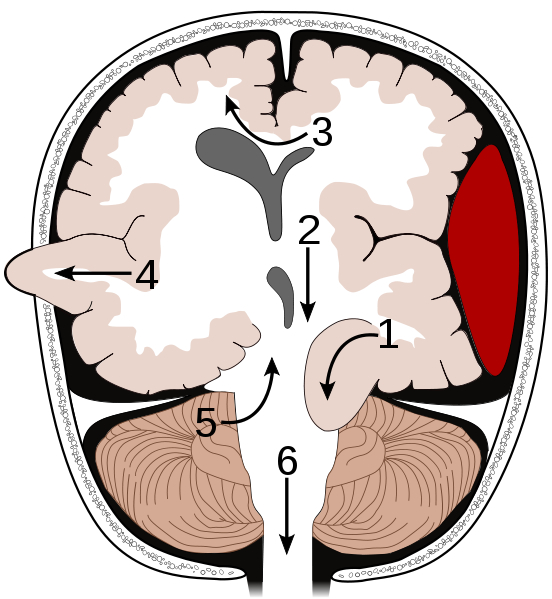
HERNIATION
• Supratentorial herniation
1. Uncal
• Infratentorial herniation
Hematomas are potentially life threatening and can cause extensive brain injury, including prolonged coma, the development of vegetative states, and even death. This is due to the effects of compression as well as secondary increases in intracranial pressure (ICP).
The brain and skull are very tightly fitted and there is little room for expansion. Hence, when blood leaks into or around the brain, something has to give and make room. Because the skull is rigid and relatively inflexible, pressure is thus exerted on the soft tissue of the brain which in turn becomes compressed.
Subfalcial herniation may occur secondary to frontal or parietal hematomas. With increased pressure in these areas the frontal-parietal areas tend to herniate medially under the falx cerebrei which separates the two hemispheres. That is, with subfalcial herniation the medial part of one frontal or parietal lobe is pushed under the falx damaging not only these regions but the cingulate gyrus.
Tonsillar/cerebellar herneation. Pressure developing from a mass lesion tends to displace the brain and in particular the cerebellum in a downward direction This also results in brainstem compression as the cerebellum is forced down in the foramen magnum.. This lead to respiratory and vasomotor abnormalities, and eventually loss of consciousness. With increasing expansion there will be respiratory arrest and death. This form of herniation can also occur secondary to an expanding fronto-temporal lobe hematoma.
COMA & LEVELS OF CONSCIOUSNESS
In general, the ability to obey simple commands is often considered as indicative of the return of consciousness. However, patients may slide in and out of consciousness and/or display fluctuating levels of awareness. That is, the patient may appear confused, stuporous, or deleterious.
Stupor. The patient is unresponsive and can only be aroused via intense, loud, or painful stimulation. They may open their eyes and in some cases make some type of verbal response only when vigrously stimulated.
Confusion. The patient has difficulty thinking in a coherent fashion and cannot carry out 2-step or complex commands. Their speech may consists of just a few words, they seem unaware of what is occurring around them and cannot grasp their immediate situation or the circumstances surrounding their condition. As such they are disoriented to time and place.
Delerium. This condition can be secondary to toxic disturbances as well as cerebral contusion. The patient is disoriented, shows fear and irritability, over-reactivity and faulty perception of sensory stimuli sometimes accompanied by visual hallucinations.
COMA
One need not actually suffer a severe head trauma in order to sustain significant damage to the brain and cognitive loss. Nor is loss of consciousness at the time of injury a prerequisite. That is, in some cases patients may experience a severe injury to the skull (e.g. depressed fracture) but only suffer mild brain damage. In contrast, a patient may seem to have sustained a mild skull injury and later demonstrate moderate to severe cognitive loss.
Nevertheless, it does appear that when a patient has lost consciousness, the longer the period of unconsciousness, the more widespread and debilitating is the injury and the loss of cognitive capability including memory functioning. However, as pertaining to mild head traumas, particularly in cases where consciousness was not lost, there simply have not been enough studies conducted by trained neuropsychologists so as to properly delineate the full potential ramifications of these injuries. Nevertheless, recent studies have indicated that significant cognitive and neuropsychological disturbances are associated with even mild injuries with no evidence of loss of consciousness (Leininger et al. 1990; Montgomery et al. 1991).
THE GLASGOW COMA SCALE.
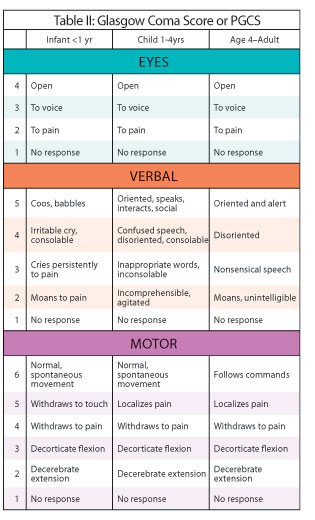
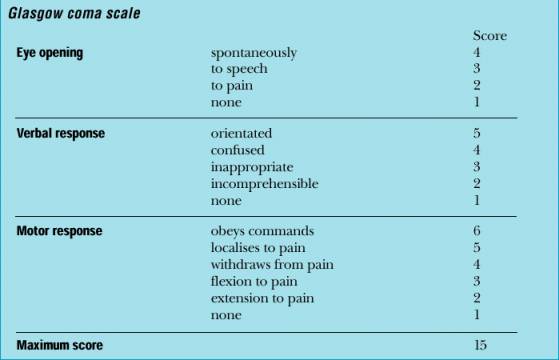
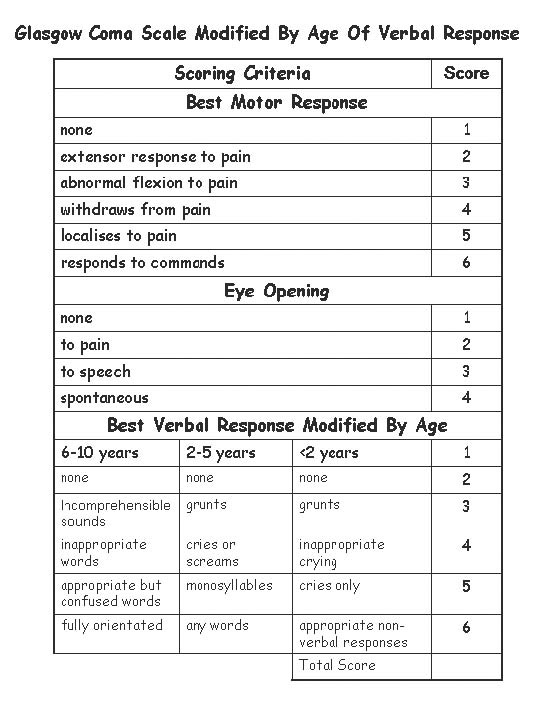
Two general indicators of severity are length of unconsciousness and extent of memory loss, both retrograde and anterograde (i.e. post-traumatic amnesia) from the time of injury. One major advance in this regard was the development of the Glasgow Coma Scale. The Glasgow Coma Scale (GCS) in effect provides standardized criteria for the assessment and description of head injury severity. Subsequently tremendous inter-rater reliability has been found in the use of this scale.
The GCS is composed of three major categories, Eye Opening, Motor Response, Verbal Response. The patients rating (or score) is based on his degree of ability to respond or react to various stimuli. If there is no response the patient receives a score of 1. Hence, the minimum score possible is 3.
Eye opening. If the patient opens his eyes spontaneously he receives a score of "4". If he opens them only in response to speech and pain, he receives a score of "3". If only in reaction to pain the score is "2".
Motor response. If the patient can adequately motorically respond to and obey commands his score is "6". If his reaction is more limited and he is capable of only responding to pain in a generalized, albeit localized manner, e.g. attempting to brush away the source, his score is "5". If he can only withdraw a limb in response to pain the score is "4". Responses limited to abnormal flexion (decorticate) are given a score of "3", whereas abnormal extensions (decerebrate) in response to pain receive a score of "2".
Verbal Response. If the patient is oriented to time, person, and place the score received is "5". Confused spontaneous verbalizations yeild a score of "4". Inappropriate verbalizations (yelling, swearing) are given a rating of "3", and incomprehensible verbalizations limited for example, to moaning, are scored "2".
SEVERITY. Hence, a patient in a vegetative coma and completely unresponsive would receive a score of "3", whereas an individual who is fully responsive and alert would receive a score of "15". On the otherhand, a patient who speaks inappropriate words, and opens their eyes and motorically withdraws only in response to painful stimuli will have a score of 9. In general, a GCS score of 8 or less is indicative of a severe head injury, 9-12 is considered moderate, and 13-15 is rated as mild.
MORTALITY
Mortality & GSC. Based on a review of a number of reports it appears that patients with a GCS score of 8 or less have a mortality rate of approximately 40% (35-50%), and that as the scores decrease the death rate increases. For example, those with a score between 3-5 have a mortality rate of approximately 60%, whereas individuals with a coma score of 6 or 7 who are between the ages of 30-50 have about a 50-50 chance of living or dying.
There is also a significantly high mortality rate for individuals who remain in a coma for 6 hours or more (Jennett et al., 1977). Indeed, in one study, of 700 such cases who were still alive 6 months after their injury, half this group died over the course of the next six months; i.e. within 1 year of injury.
In addition, the longer the coma the worse are the prospects for rehabilitation and the greater is the long term disability. Similarly, among children intellectual deficits and academic difficulties becomes more severe as coma length increases.
Mortality & Age.
Mortality (as well as severity) is also a function of age. Supposedly children suffer a lower risk of mortality from head injury as compared to adults. However, children who are physically abused, and babies who are repeatedly shaken (thus inducing brain injury; i.e. "shaken baby syndrome") are not likely to come to the attention of a physician. Nevertheless, very young children and infants have a mortality rate which is higher than older children.
In general, however, the mortality rate increases with increasing age. For example, those over 40 with severe injuries have a death rate of up to 70% whereas the mortaility rate for those below forty is 23% (Nikas, 1987). Specifically, it has been estimated that for each year over age 35, the odds of death increase by 3.6% and decrease by the same amount for each year under 35 (Teasdale et al. 1982).
Mortality & Motor Functioning. The death rate is also inversely correlated with residual motor functioning. That is, the mortality rate increases as motor function deteriorates. Disturbances in motor function are often indicative of widespread cortical or brainstem damage. Prognosis is particularly poor among those who show posturing or flaccidity of the muscles (Nikas, 1987a)
Mortality: General Complications. Complications effecting recovery and leading to mortality most commonly include hypoxia, hypotension, seizures, infections (e.g. meningitis, abscess) and unrecognized mass lesions. Indeed, many patients will talk and show some alertness after injury but due to the later development of hypoxia and associated complications, die .
The majority of patients who die, however, when first seen are often in a state of shock with subnormal blood pressure, hypothermia, fast pulse, and pale-moist skin. If this state persists along with deep coma, widely dilated pupils, no eye movements, flacid limbs, and irregular or rapid respiration, death usually follows. Hence, these are all grave prognostic signs.
At autopsy there is usually evidence of cerebral contusion. focal swelling, hemorrhage, and necrosis. A minority of such patients, however, don't die and instead persists in a state of profound disability.
VEGETATIVE STATES
Some patients will remain in a coma for months or even years and never regain consciousness. Others, however, although having suffered profound and very severe brain injuries, after a few weeks or months open their eyes and seemingly recover from their sleep-like coma, yet never truly regain consciousness . That is, recognizable mental and purposeful motor functioning never reappears. These patients are in a persistent vegetative state. Often such individual demonsrtate an absence of cortical functioning, although the lesion may be in the brainstem. In the majority of cases the brain stem is actually well preserved and it is the hemispheres and subcortical white matter which are most severely effected.
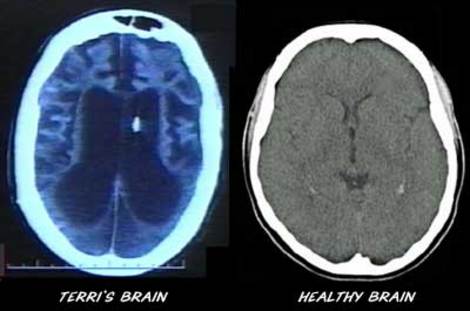
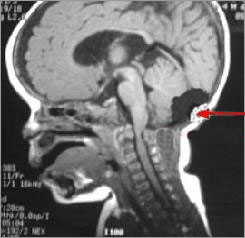
Terri Shiavo Terri Shiavo's brain.
After a few weeks these patients may open their eyes, first in response to pain, and then later spontaneously.. They may grimmice, flex the limbs or blink to threat or to loud sounds and may make roving movements of the eyes. Sometimes they seemingly follow objects and may fixate on a physician or family member. This usually gives a family member or an inexperienced physician the erroneous impression that there is cognition.
Indeed, in one case a vegatative patient was misdiagnosed as oriented to person (although she could not communicate) simply because sometimes she would open her eyes and seemingly fixate (for 1-3 seconds) on people who made sounds or called her name. However, she also would fixate on empty space and CT-scan indicated extensive and severe damage throughout the brain.
Nevertheless, among those is a vegetative state there is wakefulness without awareness and the patient remains inattentive and never speaks or gives any consistent sign indicating cognition or awareness of inner need. The limbs are often extended in a posture called decerebrate rigidity (i.e. arms and legs extended with the feet and hand internally rotated). However, after a few weeks or months this may also wear off. Sometimes there are fragments of coordinated movements that look purposeful, such as scratching, or movement toward a noxious stimulus. Patients may swallow food and water and may chew and grind their teeth for long time periods. Grunting and groaning may also be provoked thought most of the time these patients are silent. In this regard, however, their behavior is little different from that of an "anencephalic monster"; i.e. a child born with only a brainstem.
It has been argued that the term "persistent" should not be applied until at least 1 year has elapsed since injury (Berrol, 2006). This is because some patients may actually improve from the vegetative state to one of severe disability --(that is, those with traumatic vs. hypoxic damage). However, the longer the patient is in a persistent vegetative state the less potential there is for any realistic change.
2. Central (transtentorial)
3. Cingulate (subfalcine)
4. Transcalvarial
1. Upward (upward cerebellar or upward transtentorial)
2. Tonsillar (downward cerebellar)