Rhawn Gabriel Joseph, Ph.D.
BrainMind.com
CONTUSIONS, BRAIN LESIONS, & HEAD INJURIES
Following a blow to the head the skull will bend inward and sometimes strike the brain causing a contusion directly below the site of impact, i.e. a coup injury. This is because the brain, being more fluid, moves more slowly than the skull in response to force. However, except in cases of depressed skull fracture contusions are not commonly found beneath the site of impact. Indeed, damage can be widespread or localized to the contralateral half of the brain.
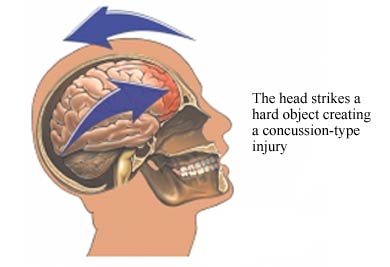

Usually the force of the impact will force the brain to shift, and/or bounce against and strike the inner bony prominences of the opposite half of the skull (i.e. contre coup injury) as well as the falx cerebri and tentorium (Leestma 2011). This results in contusions to the neocortical surface, particularly along the temporal and frontal lobes. Indeed, contusions and bruises are usually found in the orbital frontal regions and anterior and lateral temporal lobes bilaterally as well as along the convexity regardless of where the skull was struck (Adams et al., 2008). Frequently the medial portions of the brain including the corpus callosum may also be traumatized due to rotational forces such that they bump and slide against the falx and/or tentorium. In contrast, contusions are rarely encountered along the occipital lobe, even when the back of the head has been struck.
In general, contusion may consist of mutliple hemorrhages which develop immediately upon impact along the crests of the various cerebral gyri. Contusional hemorrhages may increase in size during the first few hours after injury, extending from the superficial layers of the neocortex into the white matter. Edema is usually a secondary consequence. Thus, widespread damage, varying in severity, is a likely consequence of head injury.
Necrosis.
When the brain has been contused, severely compressed, or subjected to rotational shearing forces, axons are often severed and cells crushed. This results in cell death (necrosis) within the first 24 hours after injury --a process which may continue for up to a week. After a few months time these cells are reabsorbed leaving behind glia scars and small cavities in the cortex and white matter. These scars can in turn becomes a source of abnormal activity and may cause the development of seizures.
Axonal Transport Deficits.
Trauma to the brain may interfere in axonal transport in otherwise normal neurons (see Burke et al. 2012). When this occurs there may be a buildup of neurotoxics which in turn result in cell death throughout the neuroaxis. That is, if the post-synaptic neuron is injured, axonal transport to the damaged cell may become abnormal, such that in addition to a buildup of neurotoxicity, therby giving rise to neurofibrillary tangles, amyloid plaques, and cell death.
Consciousness.
When consciousness is not lost following a head injury it is frequently erroneously assumed that the brain was not damaged. However, a patient may in fact suffer significant cognitive disturbances and extensive contusions and lacerations throughout the brain even with no loss of consciousness. Moreover, there may be complete memory for the accident with no anterograde or retrograde amnesia.
COUP & CONTRE COUP CONTUSIONS
In some instances it has been postulated that because of the differential movement of the brain there can result both coup and/or contre coup lesions. Coup contusions are due to the slapping effect of the skull hitting the brain. Tissue is damaged directly below the point of impact. Generally the head is stationary at the time of the injury.
Contre coup contusions are usually associated with translational linear acceleration injuries and the free movement of the head. Translational (linear) acceleration of the brain occurs at the moment of impact and/or as there is a rapid linear acceleration in the motion of the head --such as if thrown from a car. This causes the brain to bounce against and strike the rough bony protrusions on the opposite side of the skull.
Contre cavitation.
As pertaining to coup and contre coup lesions, rapid increases in acceleration sometimes cause the development of increased intracranial pressure at the trauma point, and decreased (contre coup) pressure at the opposite side of the cerebrum. In addition to the brain striking the opposite side of the skull, this decreased pressure at the contre coup site can cause the development of cavitation bubbles which, when they burst or callapse, cause local tissue damage, i.e. a contre coup lesion (Bakay et al. 2008). Contusions are often associated with this type of injury (Leestma 2011; Unterharnscheidt, & Sellier, 2006).
Differential effects of impact site.
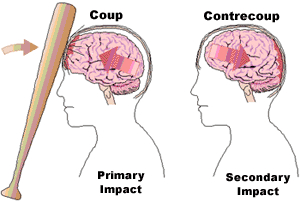
The development of coup and/or contre coupe lesions are also dependent on what part of the skull was initially impacted. That is, impact to certain regions of the skull seem to commonly result in coup lesion, whereas other zones when struck give rise to coup and contre coup damage (Leestma 2011). For example, impact at the occipital region often forces the brain to move in an anterior direction causing a contre coup lesion to the frontal lobe (Bakay et al., 2008; Lindgren, 2006). Indeed, although there is some evidence of considerable movement of the parietal-occipital region regardless of the impact site (see Bakay, Glasauner & Alker, 2008; for review), direct blows to the occiput seldom cause occipital damage.
In contrast, impact to the front of the skull almost always results in frontal lobe (coup) injuries. However, in about 50% of the cases, both coup and contre coup lesions result. Temporal impacts also create contre coup lesions. If struck from the top of the head contre coup contusions frequently develop in the corpus callosum and the orbital frontal lobes due to the downard force of the blow (Bakay et al., 2008).
Caveats.
Not all investigators accept the notion of contra coupe damage, however. Indeed, the fact that the frontal and temporal regions are most severely effected regardless of, as does the findings that when there is a skull fracture, contusion are maximal on the side of impact. Rather, it has been postulated that much of the damage which occurs secondary to impact or non-impact (including coup and contre coup) injuries are due to the effects of rotational acceleration and shearing forces.
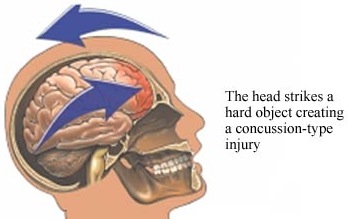
ROTATION & SHEARING FORCES
In certain types of head injuries, such as those involving a great deal of force and movement the brain will swirl, rotate, oscillate, and slosh around inside the skull in a rotary fashion. This can occur at the moment of impact or if the head is suddenly subject to rapid changes in motion (such as when the patient is air borne after been thrown through the windshield of their car vs. a blow to to the head when stationary). Indeed, rotational damage may occur even when the head has not been struck but can result from rapid skull movement alone, e.g. whiplash, severe and repeated shaking, or extreme motion of the head and neck (Adams et al. 1089; Uterharnschidt & Sellier, 2006). This is in contrast to linear acceleration injuries which are not usually associated with this differential swirling movement of the brain.

Nevertheless, as the brain swirls about the neocortical surface becomes contused, sliced and sheared by the the bony protrusions (e.g. the sphenoid wing) within the cranium and hemorrhages will develop over the surface of the cerebrum. The frontal-temporal regions are at particular risk for these type of injuries.
Brainstem & Subcortical Lesions.
However, rotational acceleration and decelerations injuries can create extensive subcortical and brainstem damage as well. For example, the cerebral hemispheres, brainstem and different parts of the brain will actually move in somewhat different directions as well as at different speeds thus inducing widespread stretching, straining and snapping of axons running throughout the white matter including the corpus callosum. Indeed, because these strains are not uniform but effect various parts of the cerebrum differently, such that one part of the brain is moving in one direction whereas another portion is sliding at a somewhat different angle, certain regions can literaly snap and break loose.
For example, when subject to severe rotational forces there sometimes is tearing at the pontine-medullary junctions (where the brainstem meets the midbrain), such that in consequence the brainstem is partly torn loose and disconnected from the rest of the brain (Hardman, 1979; Jennett & Plum, 1972). Because the cerebral hemispheres sit atop the thin brainstem, there can result torque in the pontine-midbrain junction thus disconnecting these lower from higher regions. When this occurs consciousness is lost and the patient either dies or remains in a prolonged coma.
In addition to contusions, rotational injuries are associated with venous tears, arterial shearing stresses, and hemorrhagic lesions in the midline region and throughout the brain. Nevertheless, the degree and type of damage which occurs is dependent on the speed, and direction at which the head moves. However, even presumably mild head injuries can induce brainstem injury.
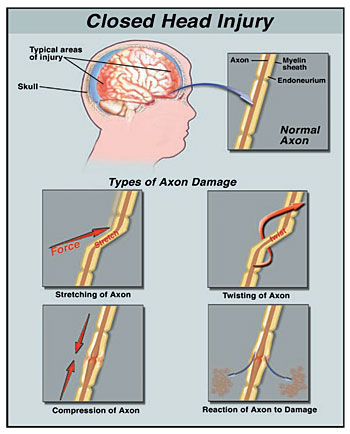
DIFFUSE AXONAL INJURY
Independent of actual impact, when the brain is subject to severe rotational and acceleration/deceleration forces, there can result severe diffuse microscopic damage and profound shearing and stretching of axons throughout the brain and brain stem as well as focal lesions in the corpus callosum. Axons are literally torn in half due to the twisting strains placed upon them. This condition is referred to as "diffuse axonal injury" (DAI).
When axons are severed or stretched the capacity to transmit electrical-chemical impulses and thus transmit information is attentuated. If severe, there can result a permanent loss of functional capabiity accompanied by an immediate and prolonged loss of consciousness. However, even in less severe head injuries subtle axonal injuries may result, including axonal swelling and impaired axonal transport and transmission (Povlishock 2012).
Conditions which give rise to DAI are also associated with brainstem damage, and decorticate and/or decerebrate posturing. When this occurs, many patients, if they survive, end up in a vegetative state. Most will die, however. If less severe there may be a temporary inability to function due to strains involving the axonal membraine (Adams et al. 1989; Gennarelli, 1986).
In general, DAI takes the form of axonal retraction balls in those who die within days, microglial scars in those who live days to weeks, as well as degneration of the fiber tracts among those who survive for longer time periods, e.g. months. That is, a few days after an injury in which axons and nerve fibers have been torn, the nerve cell often dies and the glial cellular reactions around these damaged, dying, and dead cells, creates microglia scars. Often these scars can become epileptogenic.
Moreover, because of this diffuse damage, various and widespread regions of the brain are no longer able to function or intercommunicate; i.e. disconnection. Because of this, patients with DAI who have lost consciousness yet continue to live tend not to regain consciousness but remain in a prolonged coma. Interestingly, This condition occurs more frequently among individuals who do not suffer skull fractures.