Rhawn Gabriel Joseph, Ph.D.
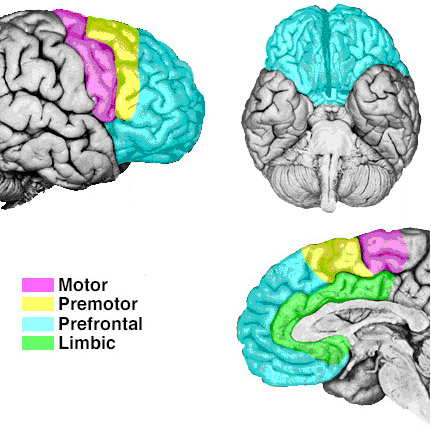
FUNCTIONAL OVERVIEW:
The right and left frontal lobes appear to exert differing influences over arousal, attention, sexual, emotional, and memory functioning (Brewer, et al., 1998; Joseph, 2007a, 1988a, 2011a; Konishi et al., 2011; Wagner et al., 1998) including even humor appreciation (Shammi & Stuss, 2011). For example, when adults who have been traumatized recall traumatic imagery of when they view combat-related photographs, the right frontal lobe displays increased activity, and the left inferior-orbital region displays reduced activity--as indicating by functional imaging and studies of cerebral blood floow (Rauch et al., 2006; Shin et al., 2007; 2011).

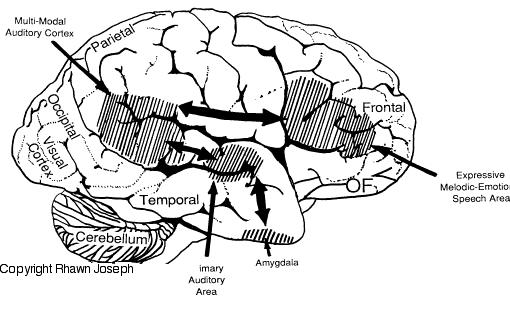
In addition, the right and left frontal lobes are lateralized in regard to language processing, with the right frontal area mediating the expression of emotional and melodic speech (Joseph, 1982, 1988a, 2011a; Ross, 1981, 1993). As is well known, the left frontal area mediates the syntactical, lexical, semantic, and temporal sequential aspects of speech. Because the right and left frontal lobe mediate different aspects of expressive speech, both areas become activated, as indicated by functional imaging, when speaking (Peterson et al., 1988). However, the left frontal lobe is clearly dominant in this regard, as is also demonstrated by functional imaging (Buchel et al., 1998; Demb et al., 2013; Demonet, et al., 2014; Gabrielli et al., 2006; Paulesu, et al., 1993; Peterson et al., 1989; Price, 2007).
On the other hand, although the left frontal lobe is dominant for speech, the right frontal lobe is dominant for arousal and appears to exert bilateral inhibitory influences over arousal whereas the influences of the left frontal lobe are more unilateral and excitatory (Joseph, 1988a, 2011a; Konishi et al., 2011; Tucker, 1981; see also Posner & Raichle, 2014). Hence, if the left frontal lobe is injured, cognitive and expressive functions tend to become suppressed and inhibited--a function not only of the injury but right frontal suppressive influences. By contrast, right frontal injuries are more likely to give rise to disinhibitory states, including the so called "frontal lobe personality"--a function in part, of loss of inhibitory influences.
Specifically, reduced speech output, Broca's aphasia, apathy, "blunted" schizophrenia and major depression are often associated with left lateral (and bilateral) frontal injuries (Bench et al., 2013; Benes, McSparren, and Bird, 1991; Buchsbaum et al. 1998; Carpenter et al. 1993; Casanova et al. 1992; Curtis et al. 1998; d'Elia and Perris 1973, Goodglass & Kaplan, 2011; Hillbom 1951; Perris 1974; Robinson and Downhill 2013; Sarno, 1998). Adults with PTSD also display reduced left frontal lobe activity (Rauch et al., 2006; Shin et al., 2007), whereas sadness can reduce right and bi-frontal activity (Mayberg et al., 2011), though in most instances depression is directly attributed to left frontal dysfunction (see below) and reduced left frontal activity as demonstrated through functional imaging (Bench et al., 2013). As per schizophrenia, it is noteworthy that lateral frontal gray matter reductions and decreased brain volume and activity have been repeatedly noted (Andreasen et al. 1990; Buchanan et al. 1998; Curtis et al. 1998).
By contrast, impulsiveness, confabulation, "motor mouth," grandiosity, and mania are often produced by right frontal (as well as bilateral) lesions (Bogousslavsky et al. 1988; Clark and Davison 1987; Cohen and Niska 1980; Cummings and Mendez 1984; Forrest 1982; Girgis 1971; Jack et al. 2003; Jamieson and Wells 1979; Joseph 2007a, 1988a, 2011a; Lishman 1973; Miller et al. 2007; Oppler 1950; Robinson and Downhill 2013; Rosenbaum and Berry 1975; Starkstein et al. 1987; Stern and Dancy 1942; Stuss and Benson 2007). Moreover, as the right frontal lobe is associated with the expression of emotional melodic speech injuries to this area can also produce pressured and/or confabulatory speech that may be melodically distorted.
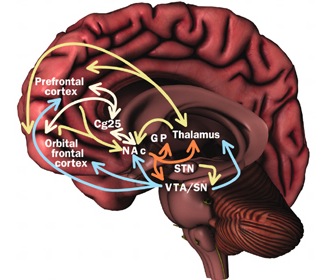
In some respects, orbital frontal dysfunction is similar to right frontal abnormalities in that patients may behave in a labile, impulsive, and emotionally inappropriate fashion. With massive injuries localized to the orbital/inferior areas, and/or which functionally disrupts the frontal-striatal pathways, patients may have difficulty inhibiting unwanted movements or thoughts, and may develop perseverative, obsessive compulsive abnormalities (Baxter et al. 1987; Breier et al. 1992; Buchanan et al. 1993; Iverson and Mishkin 1970; Luria 1980; Malloy, Birhir, and Duffy 1993; Rappoport 1991; Rauch et al. 2014; Swayze et al. 1992). In part, these gross similarities in symptomology are due to the similar role these neocortices play in regard to the control over arousal (e.g. Konishi et al., 2011; Tucker, 1981), the right frontal area regulating neocortical and thalamic activity, the orbital areas exerting inhibitory control over the limbic system (Joseph, 2011a).
By contrast, medial frontal injuries produce symptoms which in some respects are grossly similar to those associated with left frontal injuries, e.g., reduced speech output, mutism, severe apathy. With massive deep medial frontal dysfunction, the patient may become motionless, rigid, and completely catatonic (Hasslet 1980; Laplane et al. 1977; Luria 1980; Penfield & Jasper 1954; Penfield & Welch 1951). However, with less severe injuries, although suffering from disturbances of "will" and volition, patients may also develop "alien hand" symptomology, such that the right or left hand behaves in an independent and "alien" manner--sometimes completely opposite to what the patient intends.
CAVEATS: FUNCTIONAL LOCALIZATION AND SIGNATURE SYMPTOMOLOGY
As detailed below, abnormalities of and damage to the frontal lobes (vs the temporal lobe vs the striatum), can produce signature symptomology. In some cases it is possible to localize a specific subtype of schizophrenia, mania, or depression, to a specific region of the brain based upon those symptoms. Consider, for example, deficits in sacadic eye movements. Smooth pursuit and sacadic eye movements are mediated by the frontal eye fields (Braun, Boman, & Hotson, 2006; MacAvoy et al. 1991) in conjunction with the striatum, midbrain, and cerebellum. Likewise, frontal lobe deficits and reduced ability to perform frontal lobe tests such as the Wisconsin Card Sort, have been found among "Schizophrenics" with smooth pursuit and sacadic abnormalities (O'Discoll, et al. 2013; Rosse et al. 1993), whereas deficits in volitional eye movements have also been documented among those diagnosed with autism (Minshew et al., 2011)--a disorder which shares certain features with schizophrenia.
Of course, localization of pathology should be based on the entire constellation of behavioral and cognitive abnormalities, for collectively they may instead indicate a temporal rather than a frontal lobe injury, or both, and/or widespread reduction in gray matter density, increased ventricular volume, and so on (e.g. Gur et al. 1998; Harrison, 2011; Salisbury et al. 1998; Zipurksy et al. 1998). Unfortunately, psychiatric patients tend to be studied as a group based on a DSM-diagnosis, and with few exceptions (e.g. McGuire et al. 1998) are seldom selected on the basis of similarities in signature symptomology.
Moreover, because the frontal lobes receive converging input from all limbic system structures, the striatum, as well as the primary and association sensory receiving areas, in some instances deficits associated with frontal injury can be produced secondary to abnormalities in these tissues due to disconnection or abnormal activity. This has given rise to considerable confusion and a lack of consensus.
Consider, for example, schizophrenia. Whereas one group of investigators will find evidence of left frontal dysfunction or bilateral gray matter reductions, yet another will report an association with temporal lobe, or ventricular, or striatal abnormalities, whereas yet others will fail to find any clear cut associations at all (reviewed in Harrison, 2011). In consequence, there is little or no consensus as to the neurological foundations of these and other neuropsychiatric disorders, other than the fact that the brain has in some manner been compromised.
Moreover, because the frontal lobes are not a homologous structure but maintain extensive interconnections with a variety of brain regions, sometimes damage to the pathways linking the frontal lobes with these areas, or injuries to these "non-frontal" tissues, can produce similar symptoms.
For example, the caudate, putamen, and nucleus accumbens (striatum) are located in the paramedian depths of the right and left frontal lobe, and obsessive-compulsions have frequently been observed not only with frontal injuries, but in association with striatal abnormalities as based on structural (Calabrese, et al. 1993; Robinson, et al. 2013) and functional studies (Perani et al. 2013; McGuire et al. 2014).
Likewise, "schizophrenia" has been associated not only with left frontal injuries, but with left temporal (Bruder et al., 2011; Kwon et al., 2011) or left frontal-temporal lobe injuries (Harrison, 2011), or with damage to the striatum, or the frontal-striatal or temporal (hippocampal/amygdala)-striatal pathways; for example, as measured by positron-emission tomography (e.g. McGuire et al. 1998), P300 evoked potential amplitude (Bruder et al., 2011; Salisbury et al. 1998) and MRI (Jacobsen et al. 1998; Kwon et al., 2011; Nelson et al. 1998; Shidhabuddin et al. 1998), and depending on the diagnostic criteria employed. However, these tissues are functionally linked.
Similarly, mania and confabulatory delusions may be associated with right temporal, right frontal-temporal, and right frontal-parietal dysfunction (Bogousslavsky et al. 1988; Cohen and Niska 1980; Joseph 2007a, 1988a, 2011a; Robinson and Downhill 2013); depending on the diagnostic or research criterion employed as well as the nature of the lesion, e.g. stroke, vs tumor, vs seizure disorder. Again, however, these tissues are linked and often injuries are not always well localized but may compromise adjoining tissues, and even the contralateral frontal lobe--such as due to compression, seizures, etc..
Thus, where with left frontal injuries patients may seem apathetic, indifferent, and/or severely depressed and psychotic if not schizophrenic, right frontal injuries are associated with manic-like disinhibited states, including waxing and waning abnormalities associated with manic-depression. Patient's may become so disinhibited they develop the classic "frontal lobe personality," and become disinhibited, hyperactive, euphoric, extroverted, labile, overtalkative, and may develop perseveratory tendencies. Patients may become so disinhibited, delusional, grandiose, and emotionally labile that they develop what has classically been described as mania.
By contrast, with a left frontal lesion, rather than a loss of emotional control, there is a loss of emotion, and the patient will become severely apathetic, indifferent, and with massive lesions unresponsive, though classically left frontal injuries are associated with depression.
These right and left frontal differences are a function of lateralized differences in the control over arousal. Whereas the orbital frontal lobes contral limbic arousal, the right and left frontal lobes contraol neocortical arousal, with the right frontal lobe exerting bilateral inhibitory and excitatory influences, whereas the left frontal lobe exerts unilateral excitatory influences.
FRONTAL LOBE REGULATION OF THE NEOCORTEX
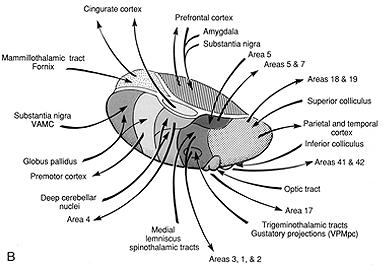
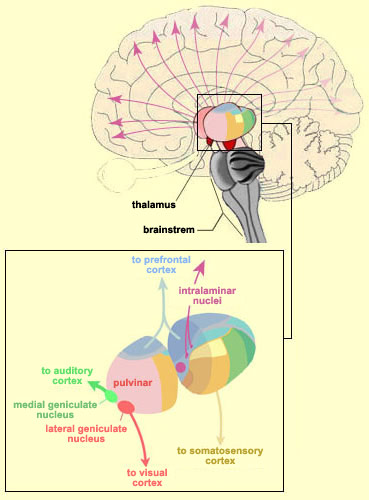
With the exception of olfactory information, which via the olfactory tracts projects to the limbic system and is relayed as well as directly transmitted to the orbital region (Cavada, 1984; Gloor, 2007), all sensory impulses are first transferred to the thalamus before being transmitted to the primary auditory, visual, and somesthetic receiving areas. From the primary zones this information is sent to 3 separate major locations: to the immediately adjacent sensory association area, back to the thalamus, and to the motor cortex of the frontal lobes.

Fibers passing to and from the thalamus and the cortical sensory receiving areas give off collaterals to the reticular thalamic nucleus--which in addition sends fibers which envelop and innervate most of the other thalamic nuclei (Scheibel & Scheibel, 1966; Updyke, 1975). The reticular thalamus maintains reccurent inhibitory interconnections with other thalamic neurons (Huntsman et al., 2011) and acts to synchronize and selectively gate transmission from the thalamus to the neocortex and continually samples thalamic-cortical activity (Skinner & Yingling, 1977; Yingling & Skinner, 1977).
Thalamic Cortical Axons
The reticular thalamus is controlled by the lateral convexity of the frontal lobes, and the lateral portion of the dorsal medial thalamus with which it maintains dense interconnections (Skinner & Yingling, 1977; Yingling & Skinner, 1977). The convexity and lateral dorsal medial nucleus (LDM) are also richly interconnected and together exert significant steering influences on the reticular thalamus. That is, the lateral frontal convexity appears to exert specific influences on the LDM so as to promote or diminish the flow of information to the cortex and thus modulate specific perceptual and cognitive activities occuring within the neocortex --activity which it is simultaneously sampling. This is in contrast to the orbital region with its connections to the reticular formation and the medial magnocellular segment of the dorsal medial thalamus, and its influences on generalized arousal and limbic activation/inhibition.
To recapitulate, the lateral frontal system is able to influence cognitive/perceptual cortical functioning via the sampling of activity occurring throughout the neocortex at all levels of informational analysis, and via its modulating influences on the lateral portion of the dorsal medial and reticular thalamic nuclei. The lateral frontal region is thus able to act at any stage of processing, from initial reception to motor expression so as to facilitate or inhibit further analysis, selectively acting to determine exactly what type of processing occurs throughut the neocortex.
Via integration and inhibitory action and through its neocortical and thalamic links the lateral convexity it is able to coordinate interactions between various regions of the neuroaxis so as to organize, mobilize, and direct overall cortical and behavioral activity and to minimize conflicting demands, impulses, distractions and/or the processing of irrelevant information.
When damaged, depending on the site (e.g. inferior vs superior convexity) or laterality of the lesion, there can result behavioral disinhibition, flooding of the sensory association areas with irrelevant information, hyperreactively, distractability, memory loss, impulsiveness, and/or apathy, reduced motor-expressive activities (e.g. speech arrest), and sensory neglect (Como et al. 1979; Fuster, 2007; Joseph 2007a, 2011a, Joseph et al. 1981; Passingham, 1993). Similar disturbances can result when the dorsal medial nucleus or the bi-directional pathways linking the thalamus and frontal lobe are severed (Graff-Radford et al.1990; Skinner & Yingling, 1977; Victor et al. 1989).
Hence, in summary, the oribtal region exerts modulating influences on subcortical and geralized limbic arousal. By contrast, the lateral convexity of the frontal lobes are "interlocked" with the the sensory receiving areas (Cavada 1984; Fuster 2007; Jones et al. 1978; Jones and Powell 1970; Joseph, 2011a; Pandya and Kuypers 1969) and maintains rich interconnections with the reticular and dorsal medial nucleus of the thalamus (Skinner and Yingling 1977; Yingling and Skinner 1977) which relays sensory impressions to the neocortex.
The lateral frontal lobes, therefore are able to sample perceptual input as it is received in the thalamus, and thus prior to and after it has been transferred to the neocortical receiving areas. Through its interconnections with the primary and association areas, the frontal lobes can also censor, inhibit, and thus control the processing of this data, and in this manner can control attention as well as facilitate or inhibit further analysis and thus information processing throughout the neocortex. These frontal capabilities include information storage and retrieval at the neocortical level; i.e. memory (Brewer et al., 1998; Carpenter et al., 2011; Hasegawa et al., 1998; Koechlin et al., 2011; Wagner et al., 1998).
In consequence, when the lateral regions are injured, selective attention and memory functioning may become impaired such that individuals may experience sensory-perceptual overload, become distractible, disinhibited, confused, and have difficulty keeping their mind on a certain tasks and/or recalling and acting upon events planned for the future. Similar disturbances can result when the dorsal medial nucleus or the bi-directional pathways linking the thalamus and frontal lobe are severed (Graff-Radford et al.1990; Skinner and Yingling 1977; Victor et al. 1989). However, the nature of these disturbances depends on if the right vs left frontal lobe has been negatively impacted.
Whereas left frontal injuries result in reduced functional and expressive activity, right frontal injuries are more likely to be associated with disinhibition, hyperreactively, distractability, impulsiveness, and the flooding of the sensory association areas with irrelevant information (Joseph 2007a, 1988a, 2011a). This is because the right frontal lobe is dominant over the left, and exerts bilateral influences in the regulation of attention and arousal (Cabeza and Nyberg 2007; DeRenzi and Faglioni 1965; Dimond 1976 1979; Heilman and Van Den Abell 1979 1980; Jeeves and Dixon 1970; Joseph 2007a, 1988ab, 2011a; Konishi et al., 2011; Pardo et al. 1991; Tucker 1981). Thus, if the left frontal lobe is damaged, the right, now acting unopposed may exert bilateral inhibitory influences and thus hypo-arousal.
THE LEFT FRONTAL LOBE:
DEPRESSION, APATHY, APHASIA, SCHIZOPHRENIA
BROCA'S EXPRESSIVE APHASIA
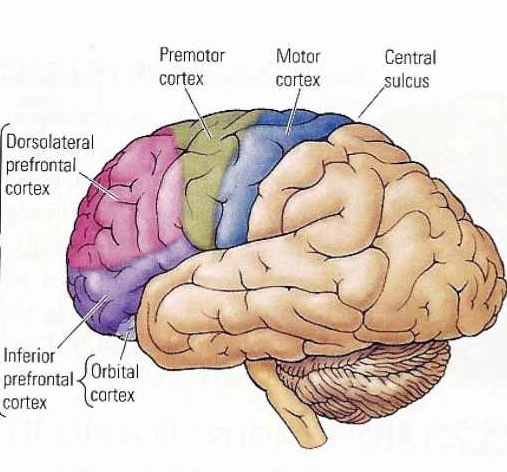
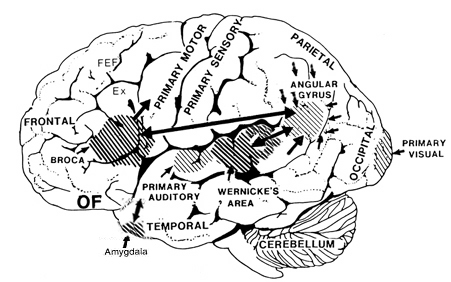
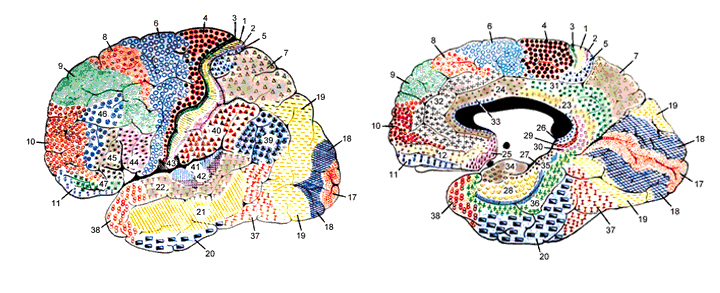
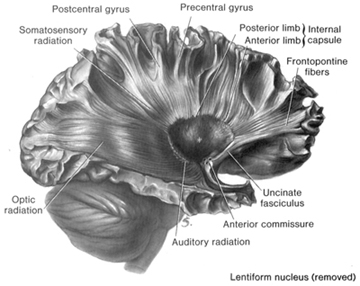
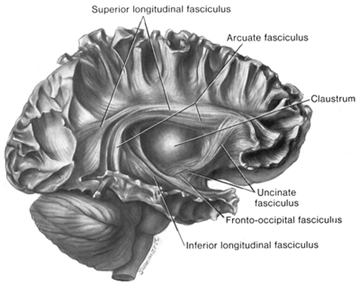
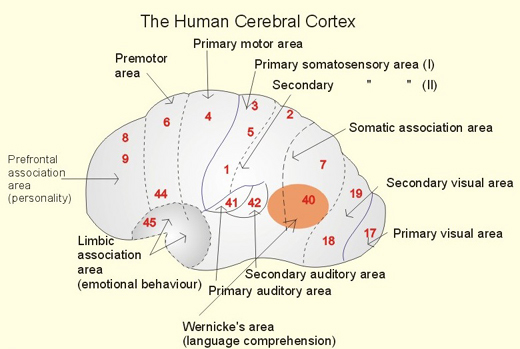
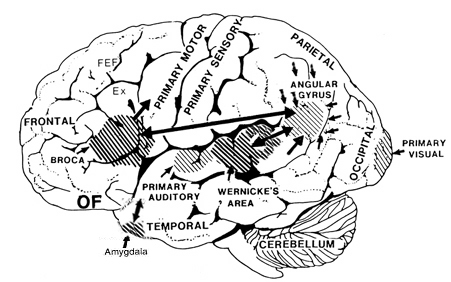
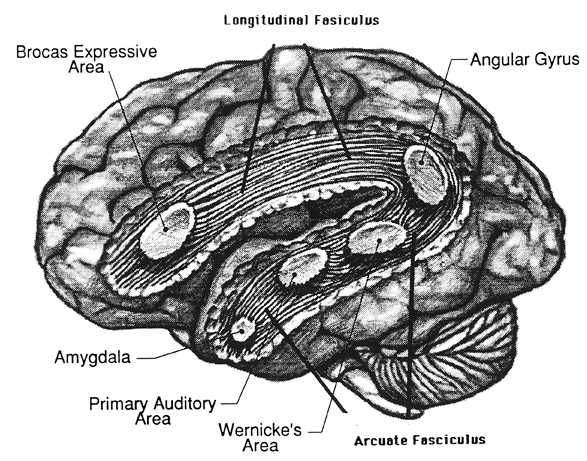
Broca's speech are is located in the general vicinity of the posterior- inferior region of the left frontal area (i.e. third frontal convolution), and includes portions of areas 45, 6, 4, and all of area 44. This region is multimodally responsive (Passingham, 2007) and receives projections from the auditory, visual, somesthetic areas (Geschwind, 1965; Jones & Powell, 1970), as well as massive input from the inferior parietal lobule and Wernicke's area via a rope of nerve fibers referred to as the arcuate fasciculus (which also links these areas to the amygdala). In addition, Broca's area receives fibers from and projects to the anterior cingulate as well as the brainstem periaqueductal gray which subserves vocalization.
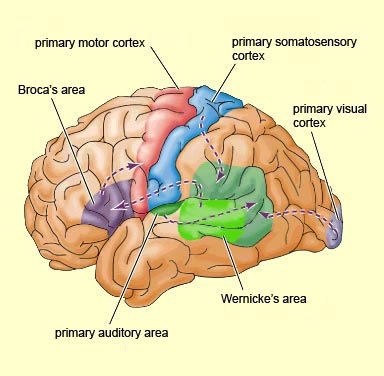
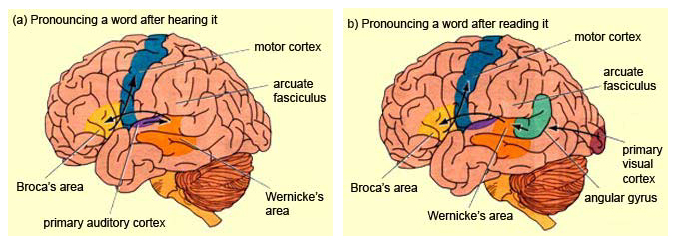
Broca's speech area is a final converging destination point through which thought and other impluses come to receive their final sequential (syntactical, grammatical) inprint so as to become organized and expressed as temporally ordered motoric articulations; i.e. speech (Foerster 1936; Fox 2013; Goodglass, 1993; Goodglass & Kaplan, 2000; Kimura, 1993; LeBlanc 1992; Petersen et al. 1988, 1990; Sarno, 1998). Verbal communication, the writing of words (via transmission to Exner's area), and the expression of thought in linguistic form is made possible via Broca's area which programs the adjacent oral-laryngeal musculature as represented within the adjacent primary motor areas (Foerster 1936; Fox 2013; Kimura, 1993; LeBlanc 1992; Petersen et al. 1988, 1990; Sarno, 1998); and which transmits to Exner's writing area so that words may be written.

The importance of Broca's area and the left frontal lobe has also been demonstrated through functional imaging. For example, the left frontal lobe becomes activated during inner speech and subvocal articulation (Paulesu, et al., 1993; Demonet, et al., 2014). The left frontal lobe also becomes highly active when reading concrete and abstract words (Buchel et al., 1998; Peterson et al., 1988), and when engaged in semantic decision making tasks (Demb et al., 2013; Gabrielli et al., 2006). Moreover, activation increases as word length increases and in response to long and umfamiliar words (Price, 2007).
With injuries to Broca's area the individual loses the capacity to produce fluent speech (Goodglass, 1993; Goodglass & Kaplan, 2000; Sarno, 1998). Output becomes extremely labored, sparse, and difficult, and they may be unable to say even single words, such as "yes" or "no". Often, immediately following a large stroke patients are almost completely mute and suffer a paralysis of the upper right extremity as well as right facial weakness (since these areas are neuronally represented in the immediately adjacent area 4). Patients are also unable to write, read out loud or repeat simple words. Interestingly, it has been repeatedly noted that almost immediately following stroke some patients will announce "I can't talk", and then lapse into frustrated partial mutism.

With less severe forms of Broca's (also referred to as expressive, motor, nonfluent, verbal) aphasia, speech remains labored, agrammatical, fragmented, extremely limited to stereotyped phrases ("yes", "no", "shit", "fine") and contaminated with syntactic and paraphasic errors i.e. "orroble" for auto, "rutton" for button (Bastiaanse, 2013; Goodglass, 1993; Goodglass & Kaplan, 2011; Haarmann & Kolk 2014; Hofstede & Kolk 2014; Levine & Sweet, 1982, 2003; Sarno, 1998; Tramo et al. 1988). Writing remains severely effected, as are oral reading and repetition. Such patients also have mild difficulties with verbal perception and comprehension (Hebben, 2007; Maher et al. 2014; Tramo et al., 1988; Sarno, 1998; Tyler et al. 2013), including the ability to follow 3-step commands (Lura 1980). Commands to purse or smack the lips, lick, suck, or blow are often, but not always, poorly executed (DeRenzi et al. 1966; Kimura 1993); a condition referred to as bucal-facial apraxia. Non-speech oral movements are seldom significantly effected (Goodglass & Kaplan, 2011; Hecaen & Albert, 1978; Kimura 1993; Levine & Sweet, 2003).
With mild damage, patients may demonstrate severe confrontive naming and word finding difficulties (anomia), as well as possible right facial, hand, and arm weakness. Speech is often characterized by long pauses, misnaming, paraphasic disturbances and articulatory abnormalities (Goodglass, 1993; Goodglass & Kaplan, 2011; Sarno, 1998). Stammering and the omission of words may also be apparent. Similarly, electrical stimulation of this region results in speech arrest (Ojemann & Whitaker, 1978; Lesser et al., 1984) and can alter the ability to write and/or perform various oral-facial movements. It is noteworthy that even with anterior lesions or surgical frontal lobectomy sparing Broca's area a considerable impoverishment of spontaneous speech can result (Luria, 1980; Milner, 1971; Novoa & Ardila, 1987).
Disturbances involving grammar and syntax, and reductions in vocabulary and word fluency in both speech and writing have been observed with frontal lesions sparing Broca's area (Benson, 1967; Crockett, Bilsker, Hurwitz, & Kozak, 2007; Goodglass & Berko, 1960; Milner, 1964; Novoa & Ardila, 1987; Petrie, 1952; Samuels & Benson, 1979; Stuss, et al., 1998; Tow, 1955). In word fluency tests, however, simple verbal generation (e.g. all words starting with L) is usually more severely impaired than semantic naming, e.g. all animals which live in the jungle--which is presumably a function of semantic processing being more dependent on posterior language areas (Stuss et al., 1998).
DEPRESSION, APHASIA, & APATHY
Depression, "psycho-motor" retardation, apathy, irritability, and blunted mental functioning are associated with neocortical injuries of the left lateral and medial frontal lobe. When Broca's area has been injured, patients not only have difficulty with expressive speech (Bastiaanse 2013; Goodglass and Kaplan 2011; Haarmann and Kolk 2014; Hofstede and Kolk 2014; Sarno, 1998) but they typically become exceedingly frustrated, irritable, and depressed (Gainnoti 1972; Robinson and Benson 1981; Robinson and Szetela 1981; Robinson and Downhill 2006).
In large part, depression is common with Broca's aphasia as patients are painfully aware of their deficit (Gainotti 1972; Joseph, 1988a). Indeed those with the smallest frontal convexity lesions often become the most depressed (Robinson and Benson 1981). Depression in these cases appears to be a normal reaction and as such is mediated by undamaged tissue; i.e., the right hemisphere which is dominant for emotional expression and perception (e.g. Borod 1992; Cancelliere and Kertesz 1990; Freeman and Traugott 1993; Heilman and Bowers 2006; Joseph 1988a; Van Strien and Morpurgo 1992). That is, the right hemisphere being emotionally astute, reacts appropriately to the patient's condition and becomes depressed. If fact, with the exception of at least one study (Mayberg et al., 2011) almost all other studies demonstrate increased right frontal activity in response to negative moods (Rauch et al., 2006; Shin et al., 2007, 2011; Teasdale et al., 2011) and decreased left frontal activity with depression (Bench et al., 2013). In fact, repetitive transcranial magnetic stimulation of the right frontal lobe reduces depressive symptoms (Klein et al., 2011), whereas left frontal activity increase with the alleviation of depression as demonstrated through functional imaging studies (Bench et al., 2013).
Not only are left frontal injuries associated with tearfulness, irritability, and depression (where it is the right which may actually feel sad), but psychiatric patients classified as depressed, and normal individuals made to feel severely depressed, demonstrate insufficient left frontal activation and arousal (d'Elia and Perris 1973, Perris 1974; Tucker et al. 1981). For example, reduced bioelectric arousal over the left frontal region has been reported following depressive mood induction (Tucker et al. 1981). Similarly depressed mothers and depressed children show reduced left relative to right frontal activation (reviewed in Dawson 2014). With recovery from depression left hemisphere arousal returns to normal levels.

Likewise, Patients who are severely depressed have been shown to demonstrate insufficient activation and a significant lower integrated amplitude of the EEG evoked response over the left vs right frontal lobe (d'Elia and Perris 1973, Perris 1974). Based on EEG and clinical observation, d'Elia and Perris have argued that the involvement of the left hemisphere is proportional to the degree of depression. Moreover, with recovery the amplitude of the evoked response increases to normal left hemisphere levels. Functional imaging of depressed states indicates reduced activity in the left frontal lobe and anterior cingulate (Bench, et al,., 1992) and when these individuals ceased to be depressed, activity levels increases (Bench et al., 2013).
Left frontal lobe depression is therefore seen in those who are aphasic, and those whose depression has been long standing or even recently provoked. The more severe the depression, the greater is the reduction in left frontal functioning (whereas with mild transient sadness there might be a reduction in right frontal activity). Hence, with massive left frontal dysfunction, including even when Broca's area is spared, patient may become exceeding depressed, apathetic , hypoactive and indifferent (Robinson et al. 1984; Robinson and Szetela 1981; Sinyour, et al. 2007). However, with severe injuries, instead of worried or emotionally depressed, the patient instead is indifferent, uncaring, apathetic, and emotionally blunted (Blumer and Benson 1975; Freeman and Watts 1942, 1943; Girgis 1971; Hecaen 1964; Luria 1980; Passingham 1993; Stuss and Benson 2007; Strom-Olsen 1946). One patient who "prior to his accident requiring amputation of the left frontal pole, had been garrulous, enjoyed people, had many friends, was active in community affairs" and had "true charisma... became quiet and remote, spent most of his time sitting alone smoking, and was frequently incontinent of urine, and occasionally of stool. He remained unconcerned and was frequently found soaking wet, calmly sitting and smoking. When asked, he would deny illness" (Blumer and Benson 1975, p. 196).
Similarly, inertia and apathy usually imediately follow surgical destruction or injury of the frontal lobes, the left frontal lobes in particular (Hillbom 1951; Lishman 1968). "The previously busy housewife who has always been a dirt-chaser, and who has kept her fingers perpetually busy with darning, crocheting, knitting, and so on, sits with her hands in her lap watching the 'snails whiz by'. Like a child she must be told to wipe the dishes, to dust the sideboard, to sweep the porch" and even then the patient completes only half the task as there is no longer any interest or initiative (Freeman and Watts 1943, p. 803). In some cases the apathy is so profound that "whoever has charge of the patient will have to pull him out of bed, otherwise he may stay there all day. It is especially necessary since he won't get up voluntarily even to go to the toilet" (p. 802).
Depressive-like features, however, also seem to result with left anterior damage sparing Broca's area such as when the frontal pole (of either hemisphere is compromised (Robinson et al. 1984; Robinson & Szetela, 1981; Sinyour, et al. 2007). As described by Kennard (1939) monkeys with bilateral frontal lobe damage would sit with their head sunk between their shoulders, neither blinking or turning their heads in response to noise, threats or the presence of intruders; but would stare absently straight ahead with no facial expression. In a similar study, following massive frontal destruction a monkey who was formerly quite active and the dominant leader of his group became inactive, indifferently watched others, failed to respond emotionally, and seemed to have lost all interest and ability to engage in complex social behavior (Batuyev, 1969).
In his summary of two large scale frontal tumor studies Hecaen (1964) noted the majority seemed confused, disorganized, apathetic, hypoactive, and suffering from inertia and feelings of indifference.However, puerility was also common among these patients and many demonstrated decreased judgment with either total or partial unawareness of the environment.
In some, this initial state of inertia disappears, whereas in others it becomes a lasting or even progressively severe disturbance. "The previously busy housewife who has always been a dirt-chaser, and who has kept her fingers perpetually busy with darning, crocheting, knitting, and so on, sits with her hands in her lap watching the 'snails whiz by'. Like a child she must be told to wipe the dishes, to dust the sideboard, to sweep the porch" and even then the patient completes only half the task as there is no longer any interest or initiative (Freeman & Watts, 1943, p. 803).
In part, depression coupled with apathy secondary to frontal injuries is probably related to damage to the interconnections with the medial region, an area which when damaged induces hypokinetic and apathetic states (see below). However, these latter patients are not depressed, but rather severly apathetic, indifferent, hypoactive, and poorly motivated. When questioned, rather than worried or truly concerned about their condition the overall picture is that of confusion, disinterest, and blunted emotionality (Freeman & Watts, 1942: Hacaen, 1964) i.e. there is a lack of worrisome thoughts or depressive ideation.
Hence, in part, apathetic and depressive features may result from left frontal convexity and frontal pole damage due to a severance of fibers which link emotional impulses (such as those being transmitted via the orbital and medial region) with external sources of input or cognitive activity which are transmitted to the convexity (i.e. disconnection), impulses which are transmitted from the medial frontal lobes to the orbital, superior, and anterior frontal lobes. Through these interconnections, emotional impulses arising in the limbic system, can be transmitted through the medial frontal lobes to the lateral frontal lobes, where they then become ideas. Or conversely, neocortical cognitions may be transmitted from the lateral neocortical surface to the medial areas where they are integrated to again become emotional ideas.
It was the recognition that the frontal lobes acted as a bridge between emotion and idea which led to the wide scale use of frontal lobotomy; i.e. surgical destruction of inter-linking fibers --a technique, which when used in the 1940s and 1950s, often involved little more than blindly swishing a "surgical ice pick" inside somebody's brain!
Moreover, convexity lesions, like medial damage, may result in a disconnection not only between cognitive-perceptual and emotional activity, but would prevent limbic system output from reaching the motor areas such that emotional-motivational impulses are unable to become integrated with motor activities. The patient is thus motorically hypo-emotionally aroused (i.e. depressed), and appears to be demonstrating psychomotor retardation. Just as left frontal convexity motor damage can result in left sided apraxia (due to right hemisphere disconnection from left parietal temporal-sequential output), the reverse can also occur. That is, with left frontal damage, linguistic impulses not only fail to become expressed, but emotional output from the right hemisphere and limbic system fail to become integrated with linguistic-ideation (i.e. thought). Ideas no longer come to be assigned emotional significance. In the extreme the motivational impetus to even engage in thought production is cut-off.
As pertaining to laterality, left frontal (vs. right) lesions are associated with reductions in intellectual and conceptual capability which often leads to confusion and a reduced ability to appreciate and appropriately respond to the external or internal environment. In these instances, one possible consequence is apathy, indifference, hyporesponsiveness, and depressive-like symptoms.
On the otherhand, it is possible that among psychiatric patients and otherwise normal, albeit, depressed individuals, that the left frontal region appears relatively inactive because the right frontal area is preoccupied with being depressed; the right frontal region is excessively aroused (Teasdale, et al., 2011). That is, excessive right frontal arousal leads to massive left frontal inhibition; i.e., the bilateral arousal system of the right hemisphere inhibiting the left.

INTELLECTUAL DEFICITS AND LACK OF CONCERN FOR LONG TERM CONSEQUENCES
It has frequently been claimed that intelligence is not effected even with massive injuries to the frontal lobes. However, this view is completely erroneous for even in mild cases, although intelligence per se may not seem to be reduced as based on IQ testing, the ability to effectively employ one's intelligence is almost always compromised.
Frontal lobe damage and lobotomy reduces one's ability to profit from experience, to anticipate consequences, or to learn from errors (Bianchi 1922; Drewe 1974; Goldstein1944; Halstead 1947; Milner 1964 1971; Nichols and Hunt 1940; Joseph 2007a, 2011a; Petrie 1952, Porteus and Peters 1947; Rylander 1939; Shallice and Burgess 1991; Stuss and Benson 2007; Tow 1955). There is a reduction in creativity, fantasy, dreaming, and abstract reasoning. The capacity to synthesize ideas into concepts or to grasp situations in their entirety is lost, and interests of an intellectual nature are diminished, or sometimes abolished. As described by Freeman and Watts (1943, p. 803) "patients who were great readers of good literature will be interested only in comic books or movie magazines. Men of considerable intellectual achievement... when discussion turns on the great events of the day will pass off some cliches as their own opinions".
In mild or severe cases thinking may be contaminated by perseverative intrusions of irrelevant and tangential ideas, randomly formed associations, and illogical intellectual activity. These patient are also often effected by the immediacy of their environment and have difficulty making plans or adequately meeting long term goals. Even if highly intelligent, they may no longer be able to use that intelligence affectively, and they may undergo a complete personality change.
In 1981, following his graduation from Stanford University, D.F., and three friends, founded their own electronics/computer company, which immediately became a modest success, and began to rapidly grow and expand. D.F., tall, lanky, clumsy, already losing his hair, and only 27 years old, was an electronics genius and in all respects the classic "nerd." He had never dated, and never had a social life, and throughout his younger years had been treated like a "retard" by his school mates. Although he was "vice president" of his company, and a co-owner, and worth over seven figures, he simply lacked the self-confidence to mingle or socialize with the opposite sex, and didn't feel comfortable interacting with anyone who did not share his enthusiasm for computers. Neverthless, D.F. was lonely. He needed a girlfriend.
In 1985 his company "went public" (made a public offering of stock) and D.F. was suddenly a multi-millionaire without a girlfriend. It was soon thereafter that a "new girl" was hired to work as an assistant and secretary, just outside his office. "She was beautiful! An angel! Long blond hair. Green eyes. She must have weighed only 100 pounds. Everytime I walked out side my office I felt shocked to see her. And she wasn't married. She was only 23. I started thinking about her all the time. I coudn't concentrate. I dreamed about her. I wanted to marry her. I loved her. Love her!" he gushed, his words racing.
But D.F. didn't have the nerve to approach her, or talk to her, except to say hi. "She always smiled at me, when I said hi. A big smile. I knew she liked me." But he still didn't ask her out. Instead, he began to fantasize, about being married, having children.
And then after several tortured months, D.F. came to a decision. "I bought her a huge diamond ring. Ten thousand dollars. And I asked her to marry me."
According to D.F., he simply approacher her, offered her the ring, which she took and put on her finger. And then he asked her to marry him. Apparently she was stunned. Apparently she even laughed. Apparently she even thanked him for the ring. But she said no.
D.F. was mortified and became massively depressed. He couldn't function. Couldn't think."I just wanted to die." D.F. purchased a handgun. Took it home. Placed the barrel in his mouth. But then aimed it incorrectly. He pointed it directly into the roof of his mouth, pulled the trigger, and then blew out his right frontal lobe.
Approximately six months later, D.F. arrived for his appointment to see me, with a toothbrush, toothpaste, hair brush, and wash rag sticking out of his shirt pocket (Joseph 1988a). When I asked, pointing at his pocket, "What's all that for?" he replied with a laugh, "That's just in case I want to brush my teeth," and in so saying he quickly drew the toothbrush from his pocket and began to demonstrate. During the course of the exam he laughingly demonstrated how the skin flap which covered the hole in his head (from the craniotomy and bullet wound) could bulge in or out when he held his breath or held his head upside down. He even climbed up and stood on this examiner's desk and bent over so as to offer a better view of the hole in his head.
Throughout the exam he behaved in a silly, puerile manner, often joking and laughing inappropriately. Even when discussing the blond secretary and the aftermath, he laughed, becoming serious for only a few moment when I asked him if she had given him back the ring. She hadn't. Nevertheless, despite his bizarre and inappropriate behavior, D.F.'s overall WAIS-R IQ was above 130 (98% rank: "Very Superior"). Unfortunately, although he had a high IQ, he could no longer employ that intelligence, intelligently. On the other hand, he was no longer depressed, which is one of the many reasons that frontal lobotomies became such a popular in-office psychiatric procedure during the 1940s and 1950s.
Frontal lobe patients also may have difficulty thinking up or considering alternative problem solving strategies and thus developing alternative lines of reasoning. For example, Nichols and Hunt (1940) dealt a patient five cards down including the ace of spades which always fell to the right on two successive deals and then to the left for two trials. The patients task was to learn this pattern and turn up the ace. The patient failed to master this after 200 trials.

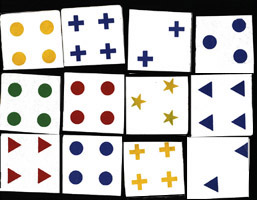
Some frontal lobe patients may also have extreme difficulty sorting even common everyday objects according to category (Rylander, 1939; Tow, 1955), for example, sorting and grouping drinking containers (glasses) with other drinking containers (mugs), tools with tools, etc. Similarily, they may have difficulty performing the Wisconsin Card Sorting Task (Crockett et al., 2007; Drewe, 1974; Milner, 1964, 1971) which involves sorting geometric figures according to similarity in color, shape, or number. However, the manner in which a patient fails on this task is dependent on the locus and laterality of the damage.
For example, patients with orbital damage seem to have relatively little difficulty performing this category sorting task (Drewe, 1974; Milner, 1971). Similarly, patients with right frontal damage, although they show a tendency to make perseverative type errors (i.e. persisting in a choice pattern which is clearly indicated as incorrect), perform significantly better than those with left frontal damage (Drewe, 1974; Milner, 1964, 1971). Thus overall, patients with left medial and convexity lesions perform most poorly, and have the greatest degree of difficulty thinking in a flexible manner or developing alternative response strategies.
I.Q. Testing
A number of studies of conceptual functioning have been performed before and after surgical destruction of the frontal lobes. Although in some cases, such as D.F., described above, the IQ remains high, performance is so uneven and there is so much intertest variability that it is apparent that patients have suffered significant declines (Petrie, 1952; Smith, 1966). In studies in which patients undergoing frontal leucotomy for intractable pain were administered the Wechsler Intelligence Scales both pre- and post surgery, a 20 point drop in the IQ was reported (Koskoff, 1948, cited by Tow, 1955).
Likewise, in cases where the Raven's Progressive Matrices or Porteus Mazes were administered both before and after lobotomy, significant declines in intellectual functioning have been documented (Petrie, 1952; Porteus & Peters, 1947; Tow, 1955). As with most tests, the usual pattern is to improve with practice. Hence, these results (and those mentioned above) indicate that frontal lobe damage disrupts abstract reasoning skills, verbal-nonverbal pattern analysis, learning and intellectual ability, as well as the capacity to anticipate the consequences of one's actions or to profit from experience. However, the effects of frontal damage on IQ is dependent on the locus of the damage.
For example, left frontal patients show lower Wechsler IQs than those with right frontal lesions (Petrie, 1952; Smith, 1966). In fact, 17 of 18 patients with left frontal damage reported by Smith (1966) scored lower across all subtests compared to those with right frontal lesions. Indeed, patients with left sided destruction perform as poorly as those with bilateral damage (Petrie, 1952).
In analyzing subtest performance, Smith (1966) notes that left frontal lobotomy patients scored particularly poorly on Picture Completion (which requires identification of missing details). This is presumably a consequence of the left cerebral hemisphere being more conerned with the perception of details (or parts, segments) vs wholes (chapters 10, 11). Petrie (1952), however, reports that performance on the Comprehension subtests (i.e. judgment, common sense) was most significantly impaired among left frontals.
In contrast, individuals with severe right frontal damage have difficulty performing Picture Arrangement--often leaving the cards in the same order in which they are laid (McFie & Thompson, 1972). This may be a consequence of deficiencies in the capacity to discern social-emotional nuances, a function at which the right hemisphere excels (chapter 10).
Nevertheless, since so few studies have been conducted it is probably not reasonable to assume that lesions lateralized to the right or left frontal lobe will always effect performance on certain subtests, particularly if there is a mild injury. It is also important to consider in what manner lateralized effects on IQ may be contributing to or secondary to reduced motivation and apathy since bilateral and left frontal damage often give rise to this constellation of symptoms. If the patient is apathetic they are not going to be motivated to perform at the best of their ability.
PSYCHOSIS & BLUNTED (NEGATIVE) SCHIZOPHRENIA
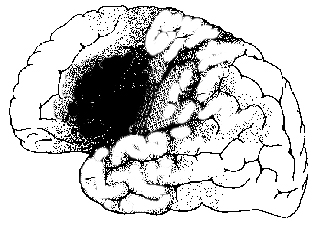
Patients with left frontal injuries or dysfunction, and who become unresponsive, apathetic, untidy, and whose speech is abnormal, are sometimes characterized as suffering from an emotionally blunted form of schizophrenia. In fact, left lateral as well as bilateral convexity abnormalities are often associated with apathetic, blunted, and "negative" forms of schizophrenia (Buchsbaum 1990; Carpenter et al. 1993; Casanova et al. 1992; Weinberger 1987; Wolkin et al. 1992). Similarly, patients classified as schizophrenic have also been reported to demonstrate abnormal left( or bilateral) frontal lobe EEG's indicative of hypoarousal (Akbarian et al. 1993; Ariel et al. 2003; Ingvar and Franzen 1974; Kolb and Whishaw 2003; Levin 1984). Lateral frontal gray matter and brain volume reductions and decreased activity have been repeatedly noted (Andreasen et al. 1990; Buchanan et al. 1998; Curtis et al. 1998), including decreased blood flow (Weinberger et al. 2007) hypoactivity (Wolkin et al. 1992), reduced metabolism (Buchsbaum et al. 1992), as well as left sided abnormalities affecting the striatum (Breier et al. 1992; Buchanan et al. 1993; Swayze et al. 1992) which is buried within the depths of the frontal lobe.
This is not to imply that all subtypes of "schizophrenia" are secondary to frontal lobe pathology. The left temporal lobe have also been implicated as measured by positron-emission tomography (e.g. McGuire et al. 1998), P300 evoked potential amplitude (Bruder et al., 2011; Salisbury et al. 1998) and MRI (Jacobsen et al. 1998; Shidhabuddin et al. 1998; Kwon et al., 2011). However, as the temporal lobes are implicated in these subtypes of schizophrenia, the pattern of symptoms differs from those with left frontal dysfunction.
For example, depending on if the right vs left and superior vs the inferior temporal lobe are more greatly impacted, patients are more emotional, more verbal, more active, and more likely to suffer visual and auditory hallucinations, coupled with disturbances of comprehension. However, whereas as a superior temporal lobe (Wernicke's area) abnormality can affect the left frontal lobe (Broca's area) thus producing fluent-aphasic speech and thus a complete formal thought disorder, left inferior temporal lobe and amygdala dysfunction can disrupt the orbital and medial frontal lobe including the caudate and putamen. Indeed, the striatum evolved from and is densely interconnected with the amygdala, and if injured mental functioning becomes invariably abnormal.
Hence, it appears that only certain subpopulations of schizophrenics actually suffer from frontal lobe dysfunction, such as those with catatonia, posturing, mannerisms, and emotional blunting coupled with reduced speech output and apathy. However, not all "frontal" schizophrenics are blunted, but may display unusual mannerisms and/or a silly, puerile childishness that long ago had been referred to as "Hebephrenia" Indeed, Hillbom (1951), described a number individuals with head trauma and missle wounds to the frontal lobes who developed schizophrenic-like symptoms, including catatonia and hebrephrenia. However, Hillbom (1951) also found that left frontal patients are more likely to develop these symptoms.
THE STRIATUM: EMOTION, PLEASURE, BODY LANGUAGE, AND SCHIZOPHRENIA
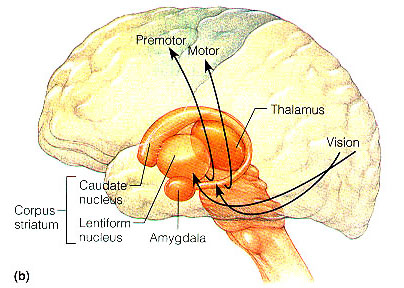
The corpus striatum (caudate and putamen) and limbic striatum (olfactory tubercle, nucleus accumbens, stria innominata) are buried deep within the frontal lobe, with the head of the caudate arising from near the orbital floor and then ascending deep alongside the inner medial and lateral walls (Mink, 2007)
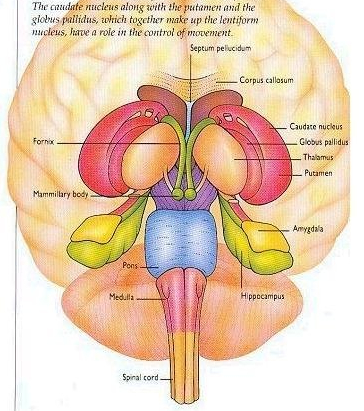
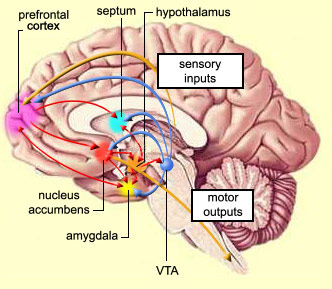
The striatal nuclei are thus intimately associated with the orbital, medial and lateral frontal lobes, as well as the amygdala with which they merge in the temporal lobe. It is through these frontal-striatal-amygdala pathways that emotional states come to translated into complex motor acts and expressed through body language (see Figure 5). That is, the striatum mediates facial expression and gesture, and produces ballistic movements, including hitting, kicking, running and biting (Mogenson and Yang 1991; MacLean 1990; Rapoport 1991).
Since humans possess basically the same striatum and limbic system, when happy, sad, angry, and so on, the facial and body musculature assumes the same readily identifiable emotional postures and expression regardless of culture or racial orgins (Ekman 1993; Eible-Ebesfedlt 1990; Joseph, 1993). The striatum is capable of considerable flexibility in motor-emotional expression, and is exceedingly responsive to the internal motivational and emotional state. Through its extensive interconnections with the limbic system and the mesolimbic dopamine (DA) system the striatum is able to perceive emotional stimuli and can "experience" pleasure. Striatal neurons selectively respond to motivationally significant stimuli that are rewarding or punishing (Rolls and Williams 1987; Schneider and Lidsky 1981) and can generate feelings of pleasure in reaction to amphetamine, cocaine and opiates (Ellison 2014; Hakan et al. 2014; Koob et al. 1991). Destruction of striatal neurons disrupts the capacity to experience pleasure such as mediated through opiates and cocaine (Koob et al. 1991).
Similarly, lesions to the corpus striatum and lenticular nucleus (putamen and globus pallidus) can attenuate one's capacity to experience pleasure or motorically express their emotions via the musculature; e.g. the face and body becomes frozen; a condition similar to Parkinson's disease. In fact, surgical destruction of or chemical lesions to the anterior corpus striatum and surrounding tissue can produce catatonic or "frozen" states, including prolonged posturing where the subjects will remain unmoving for hours, days, and even weeks at a time (Denny-Brown 1962; Spiegel and Szekely 1961).
Similar paralytic, petrified disturbances can be induced with dopamine depletion. Indeed, a major function of striatal DA is inhibition (Ellison 2014; Le Moal and Simon 1991; Mercuri et al. 1985), and DA depletion can trigger striatal as well as limbic hyperactivation (chapter 30). If hyperactivated, associated muscular activity as well as the neural pathways linking the striatum with the frontal lobe and amygdala, can be disrupted and overwhelmed, thereby giving rise to emotional and behavior paralysis. The patient may become catatonic (see below) or in the less extreme may demonstrate signs of Parkinson's disease.
Likewise, excessive DA, and reduced striatal activity can disrupt all aspects of motor, cognitive and emotional functioning, with some patients developing an acute schizophrenic psychosis (Castellanos et al. 2014; Chakos et al. 2014; Ring et al. 2014; Shihabuddin et al. 1998; Snyder 1972). In addition to reduced activity and metabolism (Buchsbaum, et al. 1992; Resnick et al. 1988; Wiesel et al. 1987), as based on MRI, limbic striatal structures are reduced in size (Shihabuddin et al. 1998) whereas the corpus striatum has been found to be increased in size in schizophrenics vs normal controls (Heckers et al. 1991; Shihabuddin et al. 1998) especially in the left hemisphere (Breier et al. 1992; Buchanan et al. 1993; Swayze et al. 1992). Moreover, as the lateral frontal neocortex is also innervated by striatal as well as DA fibers, reduced DA levels can also negatively impact the lateral frontal lobes as well as the striatum (Beatty et al. 1993).
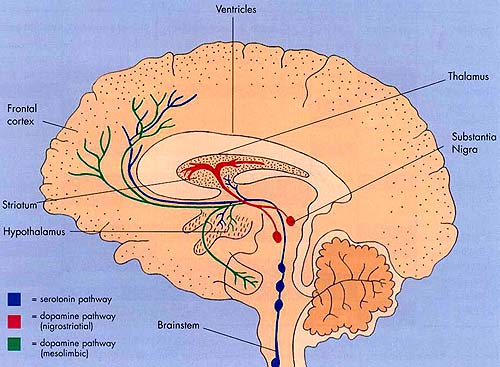
Striatal abnormalities are linked to frontal abnormalities and vice versa. In consequence, if the frontal lobes become abnormal secondary to striatal/DA disturbances, frontal symptoms will be evoked. Hence, striatal dysfunction is also associated with depression, apathy, obsessive compulsive disorders, "schizophrenia," as well as mania (Aylward et al. 2014; Baxter et al. 1992; Caplan, et al. 1990; Castellanos et al. 2014; Chakos et al. 2014; Deicken et al. 2013; Ellison 2014; Rauch et al. 2014; Richfield et al. 1987; Robinson and Downhill 2013), depending on the nature, degree, extent, and laterality of destruction.
For example, injuries or abnormalities restricted to the right caudate are more likely to result in a manic-like psychosis (Castellanos et al. 2014; Robinson and Downhill 2013) --similar to right frontal lobe injuries. By contrast, left or bilateral caudate injuries are associated with apathetic states, decreased spontaneous activity, slowed and delayed dysarthric and emotionally flat speech, with some patients responding to questions only after a 20-30 second delay (Caplan et al. 1990; Richfield et al. 1987).
For example, Richfield et al. (1987, p. 768) described a 25 year old female honor student, soon to be married, who suddenly disappeared after complaining of headaches and nausea. When found three days later she "had undergone a dramatic personality change manifested by alterations in affect, motivation, cognition, and self-care which included vulgarity, impulsiveness, violent outbursts, enuresis, indifference, hypersexuality, shoplifting and exposing herself. She was inattentive and uninterested in her surroundings. She would frequently lie down to sleep. Her affect was flat." CT-scan indicated bilateral damage to the head of the caudate nuclei as well as surrounding structures.
Since the head of the striatum descends ventrally between the lateral and medial walls, injuries to this part of the brain, including DA abnormalities, also disrupts these adjoining tissues. If the right or left lateral walls are injured, patients are likely to appear manic or apathetic, depressed, irritable, and schizophrenic. However, if the medial walls of the frontal lobes are injured, cognitive, motivational, and motor functioning will become profoundly abnormal, and the patient may become completely catatonic.
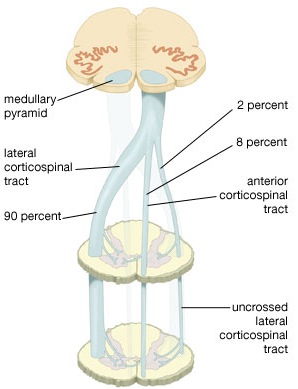
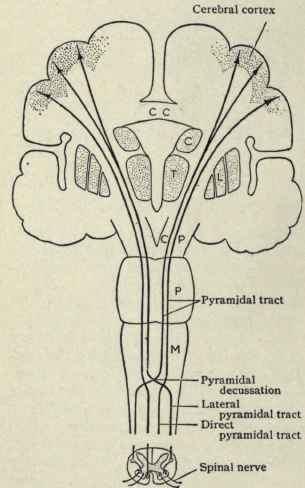
By these long descending pyramidal axons, neocortical motor control is gained via neocortical pyramidal axons which innervate the motor nuclei of the brainstem and spinal cord at all levels.
Hence, due to early left hemispheric motor development, the left corticospinal tract grows more quickly and descends into the brainstem, and then crosses at the pyramidal decussation, and then descends into the spinal cord in advance of those fibers from the right (Kertesz & Geschwind 1971; Yakovlev & Rakic 1966). This provides the left hemisphere and the right hand with a competitive advantage in establishing both motor control and thus right hand dominance.
Because the corticospinal tract does not reach advanced levels of myelination and does not become functionally mature until the 8th-12th postnatal month (Yakovlev & Lecours, 1968) it is only as the infant approaches their first birthday that handedness become obvious or apparent.
It is also around the 8th to 12th month that the motor and somatosensory areas become increasingly mature (Bell & Fox, 2014; Brody et al., 1987; Chugani, 2014; Hudspeth & Pribram, 1992; Huttenlocher, 1990; Schore, 2014) and the secondary motor and sensory receiving areas display increased myelination (Flechsig, 1901).
As based on PET scans, the frontal lobes also display increased metabolic activity from 8 to 12 months of age (Chugani, 2014), and around the end of the first year the neocortical EEG begins to increasingly resemble a more adult pattern (Kellaway, 1979; Ohtahara, 1981). In addition, around the 8th to 12th month, the corticospinal and pyramidal axons begin to approximate adult level of cellular development, myelination, and organization, and then become increasingly well myelinated over the course of the second year (Debakan, 1970; Langworthy, 1937; Yakovlev & Lecours, 1967)--a process which continues into late childhood (Paus et al., 2011).
Hence, around the 8-12th month the neocortex and frontal motor areas begin to increasingly exert hierarchical control over the limbic forebrain, brainstem, and musculature, and this process continues to develop over the course of the ensuing decade and requires considerable coordinated interaction between the parietal and motor areas of the frontal lobe as well as the striatum, limbic system, and cerebellum.
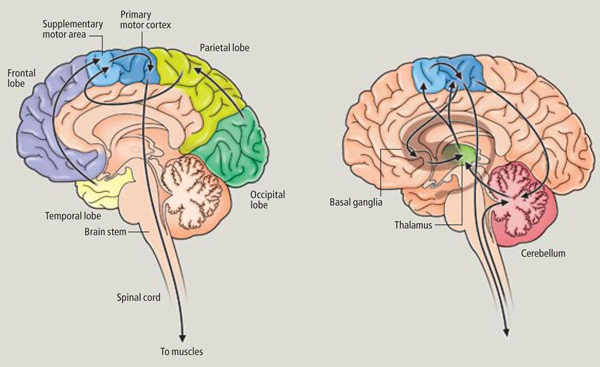
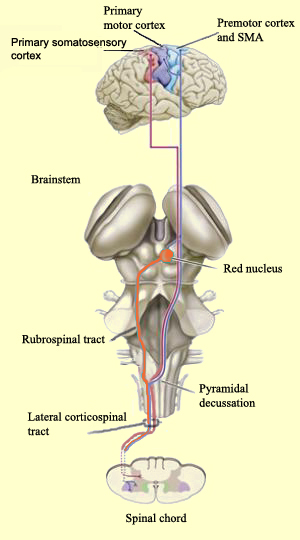
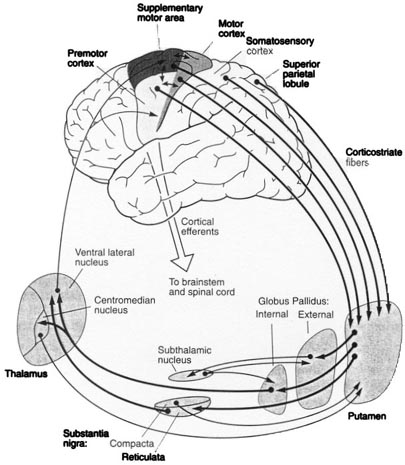
The SMA is tightly interlinked with the striatum, anterior cingulate, amygdala, as well as the motor thalamus, and contributes axons to the corticospinal tract and makes synaptic contact with the brainstem, cerebellum, and spinal cord (Brodal, 1981; Carpenter, 1991; Schmahmann, 2007). Moreover, the SMA receives input from and transmits to the premotor and primary frontal motor areas as well as from and to the parietal lobe. Hence, this structure is situated at the cross-roads where divergent impulses and sensory impression are received and apparently acts to integrate these signals. Presumably because of its integrating role, the SMA also becomes highly active during the modification, learning and establishment of new movement programs (Brinkman & Porter, 1979; Roland et al.1980; Tanji et al. 1980), and may well act to make decisions regarding possible movements based on these signals well before a movement is initiated.
In fact, single cell recordings (Brinkman & Porter, 1979; Tanji & Kurata, 1982) and studies of blood flow studies (Orgogozo & Larsen, 1979; Shibasaki et al. 1993) and movement related evoked potentials (Ikeda et al. 1992) indicate increased activity in this area when simply imagining as well as when performing complex movements of the fingers and hands.
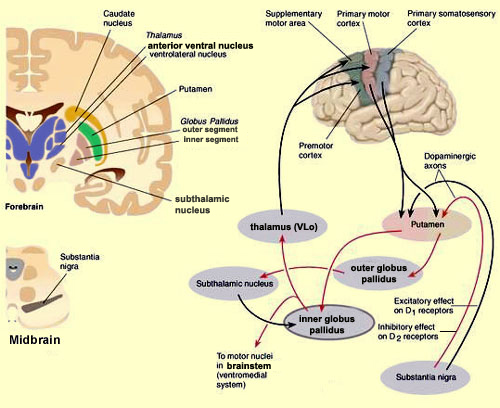
In general, however, and as based on single cell recording (vs functional imaging) activity begins in the SMA well before movements are initiated and prior to activation within the premotor and primary motor areas (Alexander & Crutcher, 1990; Crutcher & Alexander, 1990; Mink, 2007; Mink & Thach, 1991). For example, when anticipating or preparing to make a movement, but prior to the actual movement, neuronal activity will first begin and then dramatically increase in the SMA, followed by activity in the premotor and then the primary motor area, and then the caudate and last of all the putamen and globus pallidus (Alexander & Crutcher, 1990; Mink, 2007; Mink & Thach, 1991).
Presumably the putamen, in conjunction with the caudate, transmits this information to the globus pallidus which in turn projects to the motor thalamus, brainstem reticular formation, as well as to the motor neocortex, thus creating a very elaborate feedback loop (Mink, 2007; Mink & Thach, 1991; Parent & Hazrati 2013) which is also influenced by the anterior cingulate and amygdala.
The SMA, however, is not concerned with fine motor functioning, as this is the province of the primary motor areas. Rather, it is concerned with coordinating gross and bilateral movements of the hands and extremities, including grasping functions (Andres et al., 2011; Passingham, 2007; Stephan et al., 2011). Electrical stimulation of the SMA has produced complex semipurposeful movements, vocalization (Penfield & Jasper, 1954), and postural synergies involving the trunk and extremities bilaterally (Van Buren & Fedio, 1976), but not fine motor movements.
Because of its role in guiding and programming gross body movements, if this structure is damaged, the body may become stiff and movements tend to be slow and incoordinated--a condition also seen with mild lesions (Penfield & Jasper, 1954). Patients demonstrate clumsiness, severe agraphia, impairments of bimanual coordination and difficulty performing rapid or alternating movements (Brinkman, 1981; Gasquione 1993; Goldberg & Bloom 1990; Goldberg et al. 1981; McNabb et al. 1988; Penfield & Jasper, 1954; Stephan et al., 2011; Travis, 1954; Truell et al. 2013; Watson et al. 2007). Patients may walk with short steps and suffer disturbances involving posture, balance, and gait. As detailed above, with extensive and massive injuries patients may become mute (McNabb et al., 1988; Watson et al., 2007) and so stiff and unmoving that they appear to demonstrate all the classic signs of catatonia including gegenhalten and waxy flexibility.
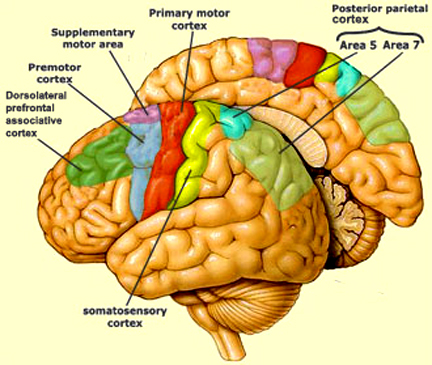
In addition to its interconnections with the SMA and primary motor areas (Jones et. al., 1978; Jones & Powell, 1970), the premotor area receives information directly from the primary and secondary somesthetic and visual (area 17, 18, 19) cortices (Jones & Powell, 1970; Pandya & Kuypers, 1969). It is precipally concerned with the guidance and refinement of movement via the assimilation of sensory information provided by the sensory areas (Godschalk et al. 1981; Porter 1990) and interacts with the basal ganglia, motor thalamus, and SMA so as to achieve these goals (Alexander & Crutcher, 1990; Crutcher & Alexander, 1990; Mink & Thach, 1991; Parent & Hazrati 2013).
As noted, the SMA becomes activated prior to the premotor area, which becomes activate prior to the primary motor area. Hence, whereas neurons in the primary motor region become active during movement, excitation in the premotor cortex precedes cellular activation of the primary region (Weinrich et al. 1984). Moreover, cells in the premotor cortex become activated before movements are even initiated, whereas electrical stimulation of this area induces the illusion of a impending movement (Penfield, 1938). These and other findings suggest that the premotor area may be modulating and exerting controlling and integrative influences on impulses which are to be transmitted to the primary region for expression.
Indeed, the premotor area appears to be highly involved in the programming of various gross and fine motor activities, and becomes highly active during the learning of new motor programs (Passingham, 2007; Porter 1990; Roland et al. 1981). Moreover, electrical stimulation elicits complex patterned movement sequences as well as stereotyped and gross motor responses such as head turning or torsion of the body (Fulton, 1934; Passingham, 1981, 1993).
Unlike the primary area, damage limited to the pre-motor cortex does not result in paralysis but disrupts fine motor functioning and dexterity, including simple activities such as finger tapping (Luria, 1980). With extensive damage fine motor skills are completely lost and phenomena such as the grasp reflex are elicited (Brodal, 1981); i.e. if the patient's hand is stimulated it will invulantarily clasp shut.
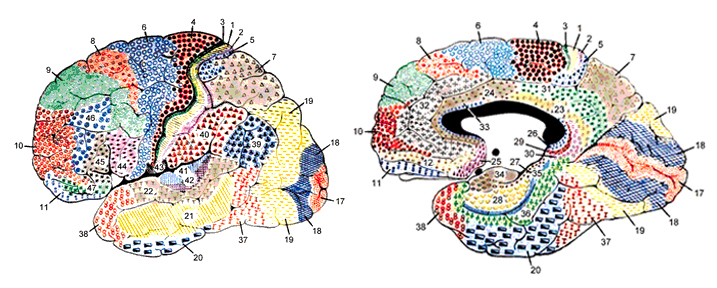
Functionally and structurally the primary motor cortex appears to extend well beyond the confines of the precentral gyrus (area 4) and includes portions of area 6 and the somatosensory (1, 2, 3, 5) regions (Brodal, 1981; Carpenter, 1991). These areas are richly interconnected (Jones et al. 1978; Jones & Powell, 1970; Kuypers & Catsamn-Berrevoets, 1984), the somatosensory projections providing information important in the sensory guidance of movement (Godschalk et al. 1981; Kaas, 1993; Lebedev et al. 2014).
As noted, axonal projections from the motor and somesthetic regions all give rise to the massive cortico-spinal (pyramidal) tract which innervates cranial nerve and sensory and spinal motor neurons (Brodal, 1981; Kuypers & Catsman-Berrevoets, 1984). For these reasons some authors have referred to the somesthetic and motor regions as the sensorimotor cortex.
The primary motor area is concerned with the coordination and expression of gross and fine motor functioning including finger movements (Colebatch et al., 1991; Luria 1980; Rao et al. 2013; Sanes et al., 2013; Shibasaki et al. 1993; Woolsey, 1958), and serves as the final common pathway where impulses organized in other brain areas are transferred for expression, particularly those involving the fingers, thumb, lips, tongue, and hand. Indeed, the region of area 4 that represents the hand is especially prominent and in fact forms a bulge upon the surface (Yousry et al., 2013).
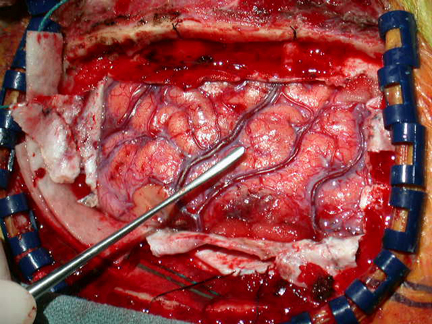
Electrical stimulation of discrete points within the motor cortex while at rest can trigger contractions and movements of tiny muscle groups on the opposite side of the body (Penfield & Jasper, 1954; Penfield & Rasmussen, 1950; Rothwell et al. 1987). Conversely, however, activation of one half of the body can induce bilateral activation of the motor area.
The primary motor area, however, is organized in a dual fashion in regard to the control over the body musculature. There is a one to one correspondence between neurons located in the primary motor area and specific muscles, which in turn makes fine motor functioning possible (Penfield & Jasper, 1954; Penfield & Rasmussen, 1950). However, there are also convergent connections as well, such that a single neuron innervates numerous muscle groups which in turn are innervated by yet other motor neurons (Humphrey, 2007; Shinoda, et al., 1981). In this manner, a neuron innervating a specific group of arm muscles, can also act on other muscles so as to coordinate movement.
Hence, a given muscle is also influenced by a number of motor neurons, such that a single muscle is represented by multiple neurons (Humphrey, 2007; Shinoda, et al., 1981). Multiple representation enables the motor cortex to coordinate a variety of movements, such that wide areas of the motor area become activated during even discrete movements of, for example a single finger (Colebatch et al., 1991; Sanes et al., 2013). Thus, activity is distributed over the motor area even when performing discrete movements.
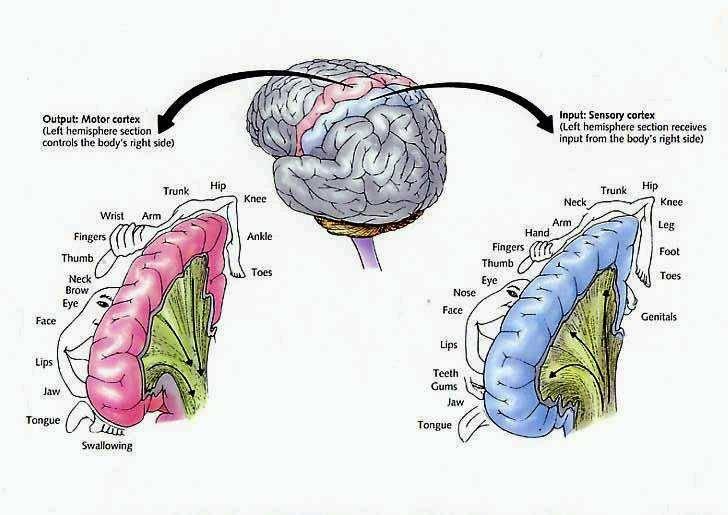
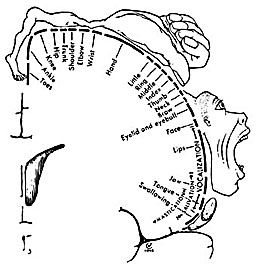
Hence, the entire musculature of the body is neuronally represented in the motor cortex. Nevertheless, since certain muscle groups play a proportionately greater role in the performance of complex (vs simple) movements, a relatively greater number of neurons are involved in their representation. Thus, the hand and fingers have extensive cortical representation (Boroojerdik et al., 2011; Penfield & Jasper, 1954; Penfield & Rasmussen, 1950; Rothwell et al. 1987) whereas a smaller neuronal field is concerned with the elbow. The motor homunculus, therefore, is quite distorted.
Specifically, represented deep in the inferior medial portion of area 4 and moving anterior toward the superior medial frontal lobe are the toes, ankle, knee, hip, anal sphincter and genitals respectively. Circling up and over the superior surface to the lateral convexity are the shoulder, elbow, wrist, and hand, with extensive areas of neocortex devoted to the fingers and thumb, followed by the brow, eyelids, larynx, lips, jaw, and tongue which is located at the most inferior opercular portion of the precentral gyrus. Like the somesthetic neocortex which maintains a double representation of the body surface (e.g. a double body image) the primary motor area contains multiple representations of the body's musculature (Colebatch et al., 1991; Humphrey, 2007; Sanes et al., 2013; Shinoda, et al., 1981).
As noted, based on single cell recording, activity begins in the primary motor area following activation of the premotor and SMA and becomes maximally active at the time of movement. However, as based on single cell recording and functional imaging, neurons in the primary motor area also become active just prior to movement, increase their activity during movement, and will become increasingly active in response to direction, velocity, and the amount of force required to perform the movement (Ashe & Gerogopoulos, 2014; Crutcher & Alexander, 1990; Passingham, 2007). Indeed, this has also been demonstrated with evoked potentials. Activity will begin in the primary motor area prior to movement, and will increase as the time of movement onset approaches, and increases in amplitude during the course of movement (Ikeda & Shibasaki, 1992). In addition, these neurons will increase their activity depending on the amount of force involved in the movement, and in reaction to the direction and velocity of movement (Ashe & Georgopoulus, 2014).
Moreover, the motor area is exceedingly plastic and as indicated above, is capable of learning and memorizing and remembering (e.g. Carpenter et al., 2011). If a single muscle is repeatedly activated and/or as an individual becomes increasingly skilled at performing a certain motor tasks, the cortical territory representing those muscles will significantly increase (Pascual-Leone et al., 2014).
Paralysis.
Damage to the motor areas, or to the descending cortico-spinal tract initially results in a flaccid hemiplegia such that the muscles are completely without tone contralateral to the lesion (Adams & Victor, 2014; Brodal, 1981). If the examiner were to raise and release an effected arm, it would drop in a limp rag doll fashion.
Over the course of the next several days the muscles develop increased tone and there is resistance to passive movements. Reflexes become very brisk and spasticity and hyperreflexia are manifest. With massive lesions extending into the medial regions (where the leg is represented), the leg will become permanently extended and the arm will assume a flexed position (Adams & Victor, 2014; Brodal, 1981). After several weeks or months a very limited capacity to perform gross movements reappears. Fine movements are usually permanently lost (Brodal, 1981).
Exner's area is dependent on Broca's expressive speech area with which it maintains extensive interconnections. In fact, Exner's writing center extends to and appears to become coextensive with Broca's area (Lesser et al. 1984)--which in turn was originally a hand area--at least in primates. Broca's area possibly acts to organize and relay impulses received from the posterior language zones to Exner's area in instances where written expression is desired. Exner's area, in turn, transfers this information to the secondary and primary motor areas for final expression.
Electrical stimulation of this vicinity in awake moving patients has resulted in the arrest of ongoing motor acts, including the capacity to write or perfrom rapid alternating movements of the fingers (Lesser et al., 1984). In some instances, writing and speech arrest were noted.
Agraphia.
Lesions or seizure activity localized to this vicinity lead to deficiencies involving the elementary motoric aspects of writing; i.e. agraphia (Penfield & Roberts, 1959; Ritaccio et al. 1992; Tohgi et al. 2013). Grapheme formation becomes labored, incoordinated, and takes on a very sloppy appearance. Cursive handwriting is usually more disturbed than printing. In cases of well circumscribed lesions, usually there are no gross deficiencies of motor functioning or speech, although mild articulatory disturbances may be observed (e.g. lisping) as well as abnormalties involving fine motor control (Cf Lesser et al., 1984; Goodglass & Kaplan, 2000; Levine & Sweet, 1982.)
In cases of pure (frontal) agraphia, spelling may or may not be affected, whereas with parietal lesions spelling as well as writing is often abnormal. Rather, with left frontal lesions more frequently there are disturbances of grapheme selection such that the patient may seem to have "forgotten" how to form certain letters and/or may misplace or even add unnecessary letters when writing (Hecaen & Albert, 1978; Tohgi et al. 2013). When spelling orally or typing the ability to spell is often better preserved.
Damage localized to this vicinity can be secondary to perinatal trauma, tumors, or vascular abnormalities. Disturbances involving constructional or manipulospatial functioning are not apparent. In fact, one such patient whose damage was secondary to birth injury, although able to write or print only with great difficulty, was able to draw and paint with some professional acumen. However, his ability to copy letters was severely effected. Hence, disturbances secondary to lesions localized to Exner's area limited to abnormalities involving linguistic-symbolic grapheme motor control.
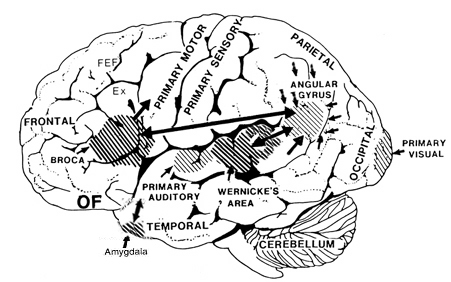
Ex=Exner's Writing Area; FEF=Frontal Eye Fields