Skull Fractures (From: Neuropsychiatry, Neuropsychology, Clinical Neuroscience, 2000, Academic Press).
Rhawn Gabriel Joseph, Ph.D.
BrainMind.com
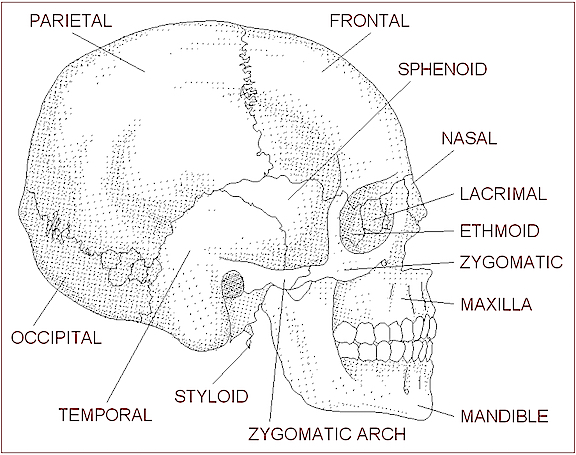
Skull fractures are of three types, depressed, linear or basilar. Basilar fracture are relatively uncommon whereas approximately 75% are linear, the remainder being depressed. In general, head injuries are also considered as either closed, or open if accompanied by scalp laceration and/or if the fracture extends into the sinuses or middle ear (Adams & Victor 2013 ).
BASILAR FRACTURES
Basilar fractures often extend into the base of the skull and are difficult to detect unless quite severe. However, existence of a basal skull fracture may be indicated by cranial nerve damage or hormonal-endocrine abnormalitiies (such as from damage to the pituitary). Fractures near the sella tursica (at the base of the skull) may tear the stalk of the pituitary such that in consequence diabetes, impotence, and reduced libido may result.
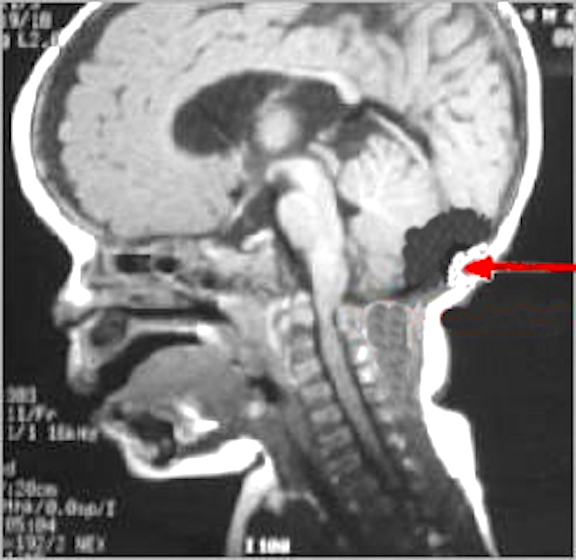
In some instances these fractures may extend in an anterior, posterior or lateral direction. If they extend in an antero-lateral direction, tearing of the olfactory, optic, oculomotor, trochlear, first and second branches of the trigeminal, and the facial and auditory nerves may occur, thus disrupting olfaction, vision, eye movements, and/or cause unilateral facial paralysis and hearing loss. If extending laterally they may damage the mastoid bone and tympanic membrane of the inner ear resulting in dizziness and disturbances involving equilibrium. and a loss of hearing.
Basilar fractures are sometimes associated with tearing of the dura as well as CSF leakage. Hence, a variety of related complications may occur including infection.
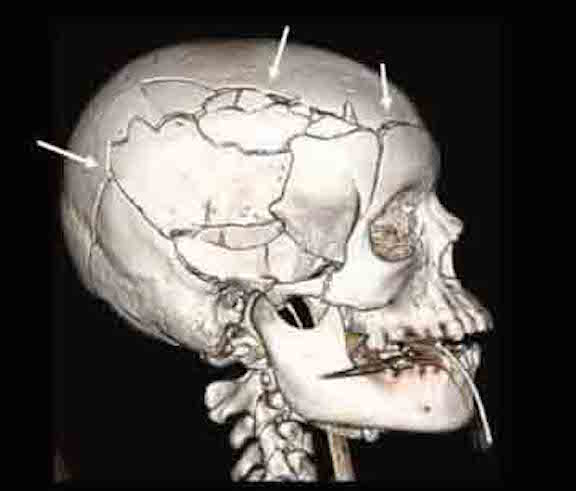
DEPRESSED FRACTURES
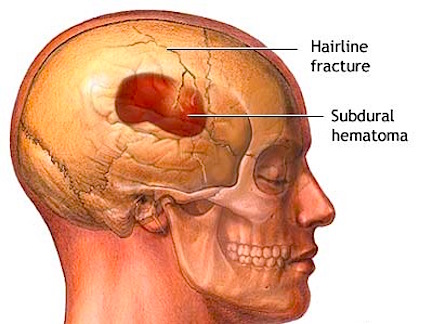
Usually with depressed fractures, part of the skull will shatter into several fragments which are driven downward toward the brain. If the dura is torn the brain is often lacerated as well. Moreover, if the dura has been torn the patient becomes vulnerable to infection, particularly in that pieces of hair or other debri may be driven into the cranial vault. This in turn will later give rise to a host of symptoms including the possible development of meningitis (Jennett & Teasdale, 2011).

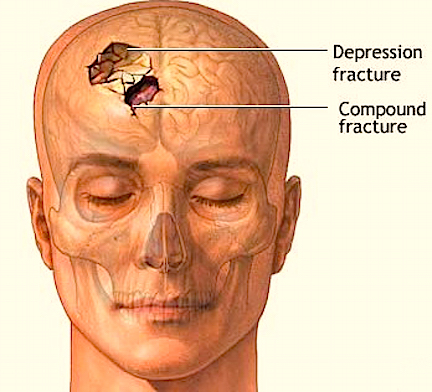
Frequently, but not always, the meningeal artery may be torn and intracerebral, extracerebral or an epidural hematomas may develop. Laceration and contusions are usually found beneath the broken bone fragments, and subdural hematomas may develop on the contralateral side (Bakay et al., 1980). If not accompanied by a laceration of the scalp, depressed fractures are described as closed.
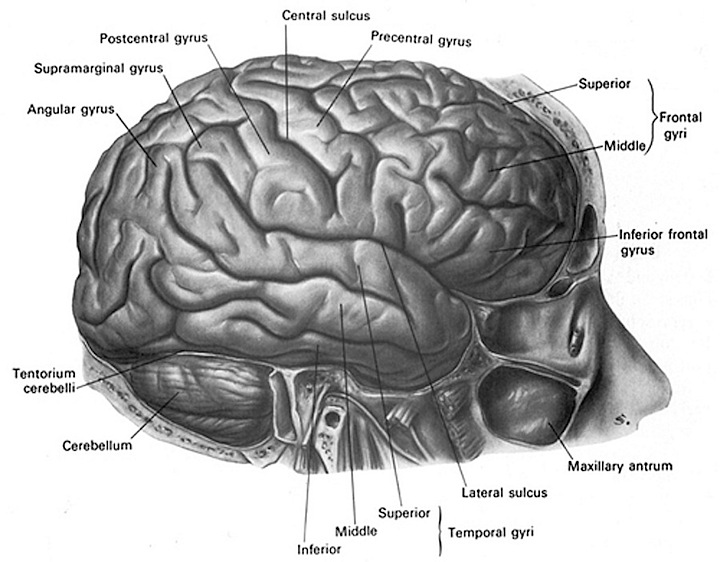
In some cases, particularly if bone fragments have been driven into the brain and/or with the development of hematomas, patients develop focal neurological signs depending on which part of the brain has been compromised.
Approximately 50% of those who suffer a depressed skull fracture do not lose consciousness (Bakay et al., 2010; Jennett & Teasdale, 2011) and in many instances the dura is spared and there is no gross evidence of neurological compromise. This does not mean, however, that the brain has not been injured.
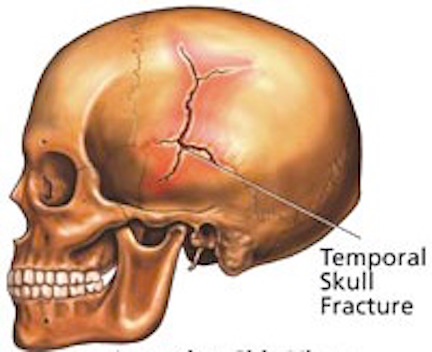
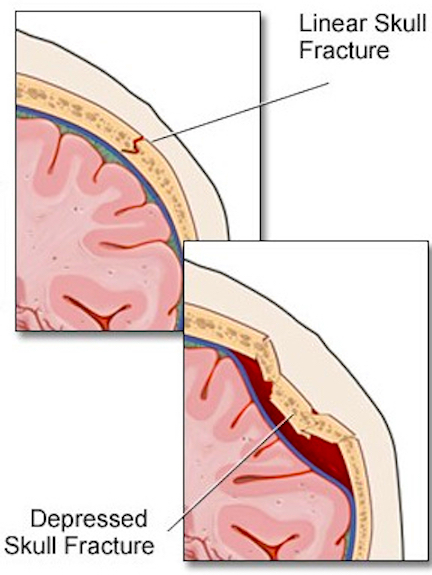
LINEAR FRACTURES
When the head is struck there usually results an inward deformation of the skull immediately beneath the site of impact whereas the surrounding area is bent outward. In some instances the skull shatters (i.e. depressed fracture) whereas in the majority of cases it will crack. Linear fractures are of two types, longitudinal and transverse.
Like depressed factures, patients may or may not lose consciousness. However, it has been reported that patients with linear fractures who retain consciousness are 400 times more likely to develop a mass lesion (e.g. hematoma) as compared to comatose patients who are 20 times more likely to develop intracranial hemorrhage (Jennett & Teasdale, 2011).
The most common sites of linear fractures involve the temporal and parietal bones. Indeed, the temporal portion of the skull may fracture following trauma to any portion of the cranium.
HEARING LOSS, VERTIGO, DIZZINESS, & BLINDNESS
Linear fractures involving the temporal-parietal bones may damage the auditory meatus, eustachian tube, and ear drum causing hearing loss, tinnitus, disorders of equiilbrium and vertigo.
Facial Paralysis.
In some instances, longitudinal fractures may damage the cochlear nucleus and cause injuries to the 7th and 5th cranial nerves which pass through this area before innervating the skin and muscles of the face. When these nerves are crushed or damaged there results a unilateral facial paralysis and loss of sensation. Transverse fractures can also cause stretching of the 7th and 8th nerves and may damage the vestibular and cochlear portions of the labyrinth. Hence, facial paralysis and hearing related abnormalities may also occur.
Anosmia.
Anosmia (loss of the sense of smell) and an apparent loss of taste (loss of aromatic flavor perception) are frequent sequala of head injury, especially following injuries to the face and fractures involving the back of the head or frontal bone. Anosmia is due to damage to the olfactory nerve, usually in the vicinity of the cribiform plate.
The cribiform plate is a wafer thin sheet of perforated bone through which the olfactory nerves pass on their journey from the nasal mucosa to the olfactory bulbs. Because this thin sheet of bone is perforated it is predisposed to fracture during head trauma regardless of where the patient was struck. This may cause the olfactory nerves to shear off thus resulting in a permanent loss of smell--anosmia. Patients are unable to even detect markedly unpleasant odors. If odors can be detected, the olfactory nerve is intact.
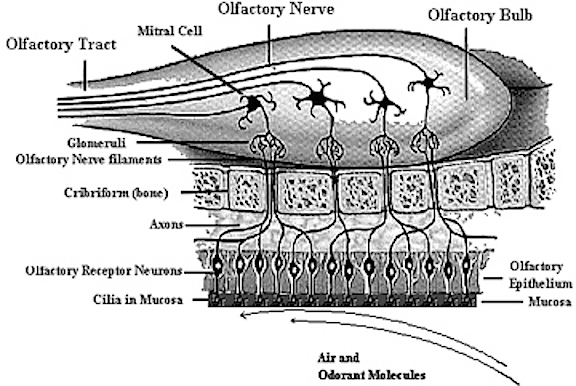
If the shearing is unilateral the loss of smell will not be recognized by the patient. It is only with complete bilateral shearing that patients begin to complain, usually noting that they have suffered a loss of taste.
With damage to the olfactory nerve and cribiform plate, sometimes there also may result a laceration or rupture of the meninges, If there is meningeal rupture cerebrospinal fluid will leak into the nose. Frequently the only symptom is what appears to be a continually "running nose". In some instances cerebrospinal fluid has gushed into the patients nose when he has coughed or sneezed --well after the injury. Hence, if a patient has a runny nose, loss of smell, but no cold or allergy, and has had a head injury, a cerebrospinal fluid fistula secondary to meningeal rupture and cribifrom plate fracture should be considered. If this is suspected he should be referred immediately to a neurosurgeon. Sometimes a secondary consequence of rupture which goes untreated is bacterial infection which may develop into meningitis.
Blindness.
Fractures near the sphenoid bone (which jutts out beneath and below the frontal bone within the skull) may result in laceration of the optic nerve. When this occurs the patient becomes immediately and permanently blind. The pupil becomes permanently dilated and is unreactive to light, although consensual reflexes are maintained. In some cases, however, an individual may be struck so hard that their eyes pop out of their sockets. In others, although the eyes do not pop out, their main be strain on the optic nerves thus causing visual problems and light sensitivity.