Rhawn Gabriel Joseph, Ph.D.
Brain Research Laboratory
BrainMind.com
EYE MOVEMENT
Movement of the eye is dependent on the functional integrity of the posterior parietal neocortex, the frontal eye fields of the lateral frontal lobes, the midbrain visual colliculi, cerebellum, and the cranial nerves and nuclei of the upper pons (cranial nerve VI) and midbrain (nerves IV & III). All pathways mediating saccadic, pursuit, and vestibulocular movements, including those originating in the forebrain and midbrain, then converge onto the pontine centers for horizontal gaze.
THE 3RD NERVE: OCULOMOTOR
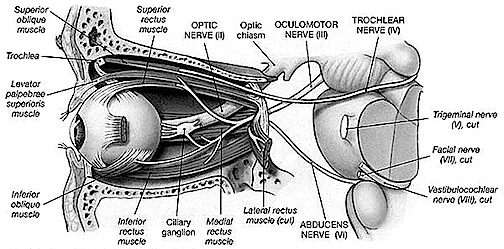
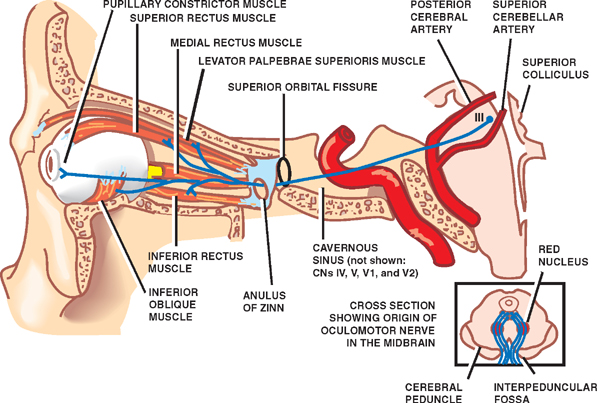
The 3rd (oculomotor) nerve is responsible for rotating the eye upward, downward, as well as inward and innervates all ocular rotary muscles (except for the lateral rectus and superior oblique). These include the medial, superior, inferior recti and inferior oblique.
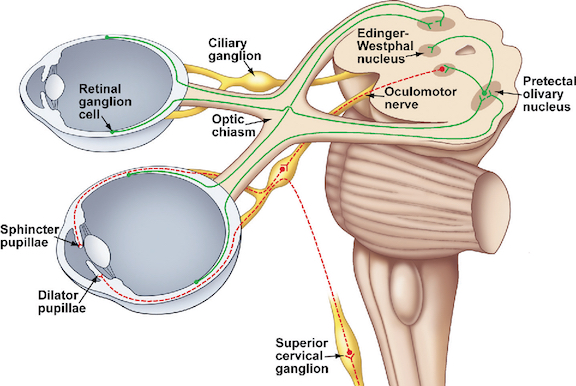
The 3rd never also innervates the intraocular and smooth muscles of the pupil; i..e. the ciliary and pupilloconstrictor muscles. Lesions, therefore, may result in an inability to rotate the eye upward, downward, or inward, and the pupil (on the side of the lesion) may fail to respond to direct light.
In addition, the 3rd nerve innervates the levator palprebrae muscle which elevates the eyelid. When the third nerve has been injured this may result in levator palpebrae weakness and thus ptosis of the eyelid.


DISTURBANCES OF EYE MOVEMENT
Eye movement nuclei are all located in the pontine brainstem and receive input from (and transmit information to) the superior (visual) colliculus within the midbrain (Grantyn & Grantyn, 1976), and the frontal eye fields (Leichnetz, et al. 1984), which also projects to the superior colliculus (Segraves & Goldberg, 1987). As is well known, the frontal eye fields and the superior colliculus become activated immediately prior to the onset of an eye movement, and stimulation of these regions elicits eye movements and visual orienting reactions as well.
Hence, damage to these cortical areas or to any of these nerves or nuclei can result in significant visual disturbances. For example strabismus (or squint) is due to a brainstem lesion that results in muscle imbalance and thus improper alignment of the visual axes of the two eyes. A complete lesion of the oculomotor nerve causes ptosis (drooping of the upper eyelid) and an inability to rotate the eye upward, downward, or inward. Lesion of the 4th nerve results in weakness of downward movement of the affected eye and patients may complain of difficulty reading or walking downstairs. Head tilting to opposite shoulder is especially characteristic. Lesion of the 6th nerve results in paralysis of lateral or outward eye movement.
Most common causes of 3, 4, 6th nerve damage are tumors of the base of the brain, trauma to head, ischemic infarction of one of these nerves, and aneurysms of the circle of Willis. Sixth nerve palsies in children are due to neoplasm-pontine glioma. The fourth nerve is most commonly injured by head trauma. Third nerve damage is often due to compression by aneurysm, tumor, or temporal lobe herniation--enlargement of the pupil is an early sign.
As noted, cranial nerves 3, 4, and 6 are linked to the 8th (vestibular) nerve via the MLF. It is due to these rich interconnections that a lesion involving these regions and the MLF can cause vertigo, dizziness, as well as nystagmus and impairment of vertical fixation and pursuit. However, disturbances such as these also raise the possibility of cerebellar dysfunction. (reviewed in Stein & Glickstein 1992).
THE OPTIC NERVE
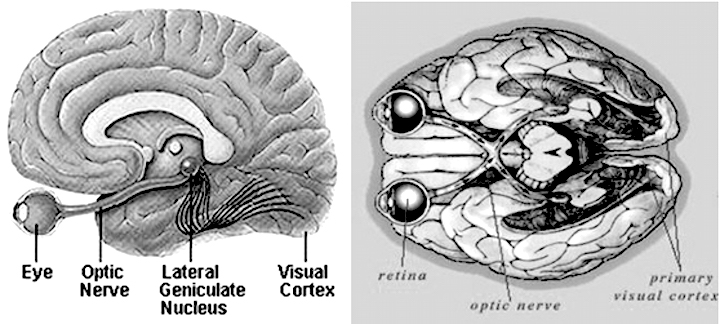
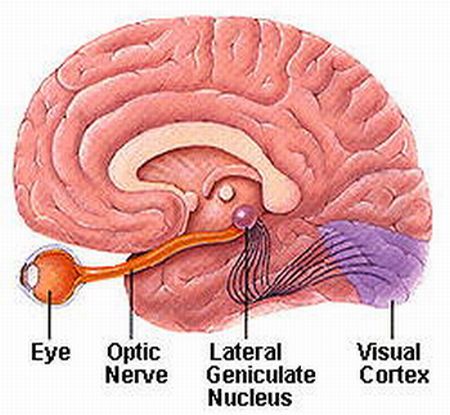
The optic nerves are responsible for transmitting all visual impulses form the retina to the brain, first crossing over at the optic chasm, and then penetrating the brain to form the optic tracts which terminate in the lateral geniculate nucleus of the thalamus. Specifically, beginning at the retina, the rods and cones project to horizontal and bipolar cells which in turn project to X, Y and W ganglion cells within the retina. Axons of the retinal ganglion cells run in parallel along the surface of the retina and converge at the optic disc (the blind spot) where they gather together and punch through the retina thereby forming the optic nerve.
The right and left optic nerves project into the cranial cavity via the optic foramina and then unite to form the optic chiasm where a decussation occurs, thereby forming the optic tracts. Subsequently, visual input from the left half of visual space projects to the right hemisphere, and input from the right half of visual space projects to the left cerebrum via the optic tracts which in turn project predominantly to the lateral geniculate nucleus of the thalamus, and to a much lesser extent, to the superior colliculus, and probably the hypothalamus, amygdala, and inferior temporal and superior parietal lobes. Because the optic nerve does not project directly to the brainstem, it is not a true cranial nerve -at least in mammals- although some fibers (via the optic tract) are received in the midbrain visual colliculi.
From the lateral geniculate nucleus these visual fibers form the optic radiations which project predominantly to the striate cortex within the occipital lobe, and give off collaterals to the inferior temporal and superior parietal lobe where the upper and lower visual fields are also represented.
Injury to the optic pathways necessarily produce visual defects and are referred to as homonymous if they are restricted to either the right or left visual field, or heteronymous if both visual fields are disrupted to some degree. Heteronymous defects suggest a lesion involving both cerebral hemispheres, or a lesion to retina or the optic nerve before it crosses over at the decussation.
If the visual defects are homonymous, then the lesion can be localized to one side of the optic tract or radiations and thus to the right or left hemisphere. Complete destruction of the optic tract or its terminal zones induces a homonymous hemianopsia to the left or right, whereas a partial injury may induce a quadratic homonymous defect: upper quadrant being associated with temporal lobe defects, and lower quadrant defects associated with the superior parietal lobe.
THE 4TH NERVE: TROCHLEAR
The 6th (abducens) nerve and nuclei are the pontine centers which control lateral eye movements outward to the right or to the left. By contrast, the 4th (trochlear) nerve and nucleus is located just caudal to the inferior colliculi, and innervates the superior oblique muscle of the eye; a muscle which has three actions: depression, abduction, intorsion. The 4th nerve therefore assists in moving the eye downward or inward.
THE SIXTH CRANIAL NERVE: ABDUCENS
The abducens is a motor nerve that innervates the lateral rectus muscle of the eye, and is part of a collection of fibers which are found with the loop of fibers that also form the facial nerve. However, fibers from the abducens nuclei also ascend the brainstem and terminate on neurons belonging to the Oculomotor complex which innervates the medial rectus muscle. It is therefore responsible for horizontal eye movements. In large part, the pontine center for lateral gaze and the abducens nuclei form a single entity (Carpenter 1991). In addition, the abducens is linked to the pontine/midbrain center for vertical gaze (the rostral interstitial nucleus of the MLF).
Thus abducens nerve and nuclei are the pontine centers which control lateral eye movements outward to the right or to the left. Injuries to the 6th nerve can therefore produce a lateral gaze paralysis as well as a paralysis of the lateral rectus muscle which results in double vision (horizontal diplopia).